无声的苦难:亚太地区罕见病 的认知与管理评估
随着亚太地区打算开始掌控罕见病这项社会议题,接下来将有许多重大且不断浮现的挑战需要应对。 虽然医疗与社会系统在许多层面有相当的进展,但仍有许多问题有待解决。
本次由杰特贝林CSL Behring公司赞助经济学人智库的研究将着眼于亚太地区罕见病所面临的困境、五个经济体如何准备应对这一挑战,并回顾各国相关措施如何为罕见病提供更好的医疗服务。 本报告汇整并分析了涵盖500多名临床医生的大量调查数据,以及与16位研究、医疗、政府和病友组织方面的专家的访谈,并进行了广泛的案头研究。
2019年11月至12月,经济学人智库(The Economist Intelligence Unit)访问了五个亚太市场的503名医疗专业人员,以评估他们对罕见病的了解,并找出地区医疗系统所面临的挑战。 受访者包括执业中的专科医生(n=172名)、基层医疗医师(n=229名)、护
士(n=40名)及药师(n=62名) 。 受访市场包括澳大利亚(n=103)、中国大陆(n=100)、日本(n=100)、韩国(n=100)和台湾 (n=100)。此外,我们与16名来自临床与病友组织的专家代表进行了深入情境式访谈,从而为本研究计划和这份报告提供了参考。 我们诚挚地感谢以下人员的参与及洞见:
Related content

Suffering in silence: Assessing rare disease awareness and management in As...
As the region begins to get to grips with rare diseases, it will need to address significant challenges, some of which are still emerging. Health and social systems are making progress in many of these areas, but finding solutions remains a work in progress.
This Economist Intelligence Unit study, sponsored by CSL Behring, looks at the nature of the rare disease challenge in the region, how prepared five of its economies are to face it, and reviews the initiatives aiming to provide better care. It draws on a substantial survey of over 500 clinicians, interviews with 16 academic, medical, government and patient experts, and extensive desk research.
In November-December 2019, The Economist Intelligence Unit surveyed 503 healthcare professionals across five Asia-Pacific markets to gauge their understanding of rare diseases and identify the challenges faced by national health systems. Respondents comprised currently practicing specialist physicians (n=172), general practitioners (n=229), nurses (n=40) and pharmacists (n=62). Markets included were Australia (n=103), China (n=100), Japan (n=100), South Korea (n=100) and Taiwan (n=100).
In addition, in-depth contextualising interviews were conducted with 16 expert representatives of clinical practice and patient organisations to inform our research programme and this report. Our sincerest thanks go to the following for their time and insight:
Takeya Adachi, program officer, Agency for Medical Research and Development, Japan Younjhin Ahn, Division of Rare Diseases, Korean National Institute of Health Centre for Biomedical Sciences, South Korea Matthew Bellgard, professor and director of eResearch, Queensland University of Technology, Australia and chair of the Asia Pacific Economic Cooperation (APEC) Rare Disease Network, Australia Gareth Baynam, clinical geneticist and director of the Undiagnosed Diseases Program Genetic Services of Western Australia, Australia Dong Dong, research assistant professor, Chinese University of Hong Kong, Hong Kong SAR Elizabeth Elliott, professor of Paediatrics and Child Health, University of Sydney, Australia Kevin Huang, founder, Chinese Organization for Rare Disorders, China Ritu Jain, president, Asia-Pacific Alliance of Rare Disease Organisation, Singapore Sonoko Misawa, associate professor, Chiba University Graduate School of Medicine, Japan Yukiko Nishimura, founder and president, NPO ASrid (Advocacy Service for Rare and Intractable Diseases’ Multi-Stakeholders in Japan) Min-Chieh Tseng, co-founder, Taiwan Foundation for Rare Diseases, Taiwan Gregory Vijayendran, chair, Rainbow Across Borders Richard Vines, chair, Rare Cancers Australia, Australia Jiaan-Der Wang, director of the Centre for Rare Diseases and Haemophilia, Taichung Veterans General Hospital, Taiwan Yi’ou Wang, secretary-general, Illness Challenge Foundation, China Chao-Chun Wu, deputy director general, Health Promotion Administration TaiwanThis research project was sponsored by CSL Behring. This report was written by Paul Kielstra and edited by Jesse Quigley Jones of The Economist Intelligence Unit.
Other language versions:
Snapshots:
Australia | China | Japan | Korea | Taiwan
无声的苦难:中国大陆罕见病的认知与管理评估
日本における希少疾患の現状: 認知度・QoL向上に向けた課題と取り組み
침묵 속의 고통: 한국의 희귀질환 인 식 및 관리현황 평가
無聲的苦難:評估台灣對於罕見疾病之認知與管理
Video highlights:
English | Simplified Chinese | Japanese | Korean | Traditional Chinese

Suffering in silence: Assessing rare disease awareness and management in Au...
In November-December 2019, The Economist Intelligence Unit surveyed 103 practising healthcare professionals from Australia, as part of an Asia-Pacific analysis of understanding and challenges faced in managing rare diseases.
Our survey respondents from Australia comprised general practitioners or primary care physicians (45.5%), specialist physicians (34.2%), nurses (8.0%) and pharmacists (12.3%). Respondents predominately worked in private (49.7%) and public or teaching healthcare institutions (46.5%).
Full reports:
Snapshots:
Australia | China | Japan | Korea | Taiwan
无声的苦难:中国大陆罕见病的认知与管理评估
日本における希少疾患の現状: 認知度・QoL向上に向けた課題と取り組み
침묵 속의 고통: 한국의 희귀질환 인 식 및 관리현황 평가
無聲的苦難:評估台灣對於罕見疾病之認知與管理
Video highlights:
English | Simplified Chinese | Japanese | Korean | Traditional Chinese

Suffering in silence: Assessing rare disease awareness and management in Ja...
In November-December 2019, The Economist Intelligence Unit surveyed 100 practising healthcare professionals from Japan, as part of an Asia-Pacific analysis of understanding and challenges faced in managing rare diseases.
Our survey respondents from Japan comprised general practitioners or primary care physicians (44%), specialist physicians (35%), nurses (6%) and pharmacists (14%). The majority of respondents reported working in private (64%) and public or teaching healthcare institutions (16%).
Full reports:
Snapshots:
Australia | China | Japan | Korea | Taiwan
无声的苦难:中国大陆罕见病的认知与管理评估
日本における希少疾患の現状: 認知度・QoL向上に向けた課題と取り組み
침묵 속의 고통: 한국의 희귀질환 인 식 및 관리현황 평가
無聲的苦難:評估台灣對於罕見疾病之認知與管理
Video highlights:
English | Simplified Chinese | Japanese | Korean | Traditional Chinese
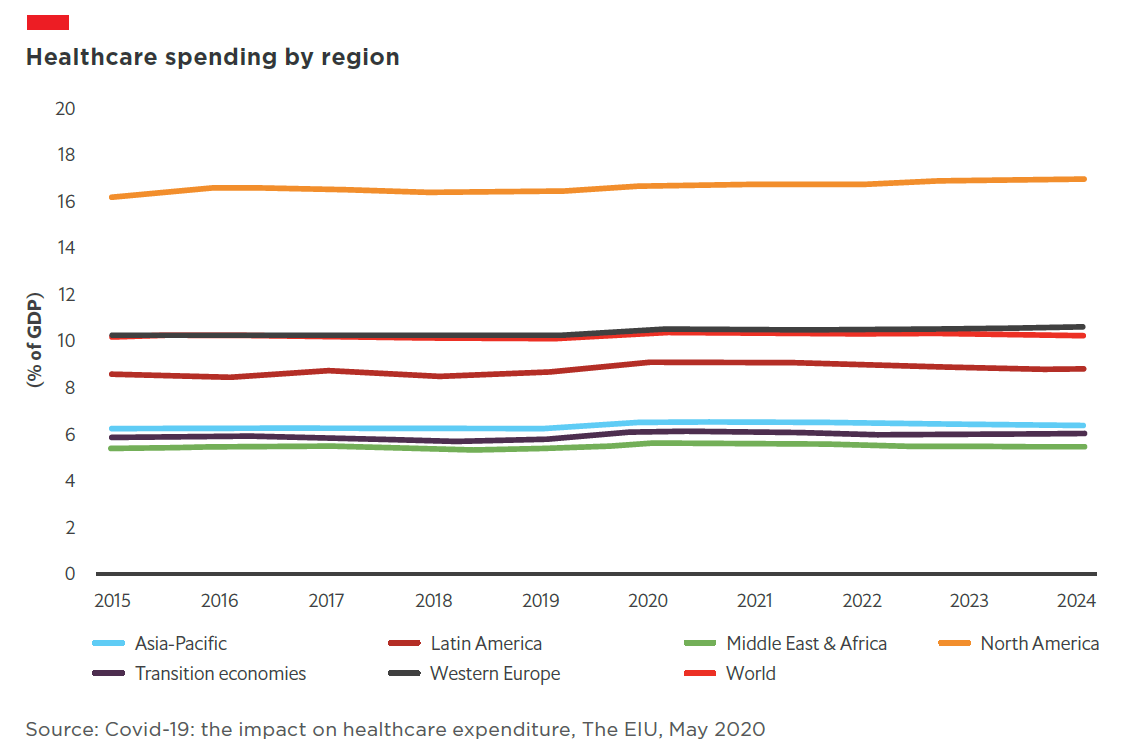
Healthcare | How will covid-19 reshape key Australian industries?
On March 11th 2020, the Australian federal government announced a A$2.4bn (US$1.6bn) funding injection into the healthcare sector to help states and territories cover the public health costs associated with treating covid-19 cases. The overall strategy was to minimise the number of people becoming sick and dying from covid-19 as well as managing the demand on Australia’s health systems.
17431
Related content

Financing sustainability: Asia Pacific embraces the ESG challenge
Financing sustainability: Asia Pacific embraces the ESG challenge is an Economist Intelligence Unit report, sponsored by Westpac. It explores the drivers of sustainable finance growth in Asia Pacific as well as the factors constraining it. The analysis is based on two parallel surveys—one of investors and one of issuers—conducted in September and October 2019.
If the countries of Asia Pacific are to limit the negative environmental effects of continued economic growth, and companies in the region are to mitigate their potential climate risks and make a positive business contribution through improving the environment and meeting the UN's Sustainable Development Goals (SDGs), large volumes of investment in sustainable projects and businesses need to be mobilised. A viable sustainable finance market is taking shape in the region to channel commercial investor funds, and both investors and issuers say they are achieving a financial benefit from their investment and financing activities. The market is still in the early stages of development, however, and must expand and mature to meet investor needs.
The chief constraint on sustainable finance growth in the region has been the limited supply of bankable sustainable projects. Our research suggests supply is increasing, but with investor demand continuing to grow apace, the gap will remain an obstacle in the short- to medium-term. Among the organisations in our issuer survey, only 7% have used sustainable finance instruments to fund projects. However, nearly nine in ten (87%) said they intend to do so in the next year, which should begin to bridge the gap between supply and demand.
Based on issuers’ stated intentions, investors will have a range of instruments to choose from, including green loans and bonds and sustainability loans and bonds. Large numbers of investors indicate that they intend to deploy a greater proportion of capital to these over the next three years.

Financing sustainability | Insights video
What is driving the strong demand for financing sustainability in Asia Pacific? How can companies increase supply and start to see the benefits of sustainable finance in the next three years? We interviewed Richard Brandweiner, CEO of Pendal Australia, and Sophia Cheng, CIO of Cathay Financial Holdings and chair of Asia Investor Group on Climate Change, to find out.
To learn more: Download report | View infographic
Financing sustainability | Infographic
Financing sustainability: How do investors and issuers in APAC's sustainable finance market view the present market opportunities and constraints?
To learn more:
Download report | Watch videoDavid Miliband: International political response to covid-19 scores “D-minus”
David Miliband is taking refuge in North-west Connecticut during the covid-19 lockdown, but his thoughts are very much global, and inevitably political.
17412
Related content

Covid-19 population tracker: deaths from covid-19 and the ones we must not...
There has been a morbid fascination with the number of deaths associated with covid-19 and the extent to which countries are mishandling the crisis. But we are also facing a data crisis which distorts proper analysis of either.
Scientists are tinkering with models on the expected number of deaths based on incomplete data as not all countries apply the same covid-19 testing rules and not all deaths are accurately recorded. At the same time countries are still deliberating about who they should test, be it asymptomatic cases, only those with symptoms, those presenting to healthcare systems or healthcare workers.
Officials in the US have cast doubt on the numbers being reported by China, and not all countries have the resources to follow the WHO’s “test, test, test” advice. This is particularly true for economies with under-developed healthcare systems such as India, Africa and Latin America.
So with that cautionary note, we have tried to work with the data at hand—incomplete as it is—to map the number of confirmed cases of covid-19 against deaths per 100,000 population over time. While the absolute numbers of deaths are important to note because each loss of life is painful to loved ones, we should also look at death rates across populations to better understand the virus and to keep abreast of potentially effective containment measures. In developing countries cause of death information is often hard to obtain, mostly because systems for recording these details are inadequate or non-existent.
The bubbles represent absolute deaths in an individual country. You can eliminate regions from the timeline to see, for example, how Europe is faring against North America, or zoom in on the trajectory for an individual country. As of April 20th, death rates appear to be highest in Europe with Belgium reaching around 50 deaths per 100,000 population.
While people are still focused on covid-19 deaths, be prepared for a new type of death associated with covid-19 over time. These are deaths and morbidity that will arise as healthcare systems direct more and more resources to covid-19 and less and less to common diseases such as stroke and cancer. For developing countries, the common diseases affected will be tuberculosis, malaria and AIDS.
These “excess” deaths may also arise as people become more fearful of overloading healthcare systems or worried about catching the virus if they attend healthcare facilities including hospitals. There are also the deaths of older people living in residential care facilities or dying at home that are not being properly accounted for. If you have cancer and your treatment is delayed, that is a life and death situation for your overall prognosis. The same applies if treatment is delayed following the first signs of stroke. Patients living with chronic health conditions will see a significant change in the level of service and care received during this crisis, and the damage caused may take years to repair.
So while scientists study the data around covid-19, expect new data to emerge on how other diseases have been affected by this pandemic.

Value-based healthcare in Sweden: Reaching the next level
The need to get better value from healthcare investment has never been more important as ageing populations and increasing numbers of people with multiple chronic conditions force governments to make limited financial resources go further.
These pressures, along with a greater focus on patient-centred care, have raised the profile of VBHC, especially in European healthcare systems. Sweden, with its highly comprehensive and egalitarian healthcare system, has been a leader in implementing VBHC from the beginning, a fact that was underscored in a 2016 global assessment of VBHC published by The Economist Intelligence Unit.
This paper looks at the ways in which Sweden has implemented VBHC, the areas in which it has faced obstacles and the lessons that it can teach other countries and health systems looking to improve the value of their own healthcare investments.
Covid-19 population tracker: deaths from covid-19 and the ones we must not forget
There has been a morbid fascination with the number of deaths associated with covid-19 and the extent to which countries are mishandling the crisis. But we are also facing a data crisis which distorts proper analysis of either.
17404
Related content

Value-based healthcare in Sweden: Reaching the next level
The need to get better value from healthcare investment has never been more important as ageing populations and increasing numbers of people with multiple chronic conditions force governments to make limited financial resources go further.
These pressures, along with a greater focus on patient-centred care, have raised the profile of VBHC, especially in European healthcare systems. Sweden, with its highly comprehensive and egalitarian healthcare system, has been a leader in implementing VBHC from the beginning, a fact that was underscored in a 2016 global assessment of VBHC published by The Economist Intelligence Unit.
This paper looks at the ways in which Sweden has implemented VBHC, the areas in which it has faced obstacles and the lessons that it can teach other countries and health systems looking to improve the value of their own healthcare investments.

Breast cancer patients and survivors in the Asia-Pacific workforce
With more older women also working, how will the rising trend of breast cancer survivorship manifest in workplace policies, practices and culture? What challenges do breast cancer survivors face when trying to reintegrate into the workforce, or to continue working during treatment? How can governments, companies and society at large play a constructive role?
This series of reports looks at the situation for breast cancer survivors in Australia, New Zealand and South Korea. It finds that while progress has been made, more needs to be done, particularly in South Korea, where public stigma around cancer remains high.
The Cost of Silence
Cardiovascular diseases levy a substantial financial toll on individuals, their households and the public finances. These include the costs of hospital treatment, long-term disease management and recurring incidence of heart attacks and stroke. They also include the costs of functional impairment and knock-on costs as families may lose breadwinners or have to withdraw other family members from the workforce to care for a CVD patient. Governments also lose tax revenue due to early retirement and mortality, and can be forced to reallocate public finances from other budgets to maintain an accessible healthcare system in the face of rising costs.
As such, there is a need for more awareness of the ways in which people should actively work to reduce their CVD risk. There is also a need for more primary and secondary preventative support from health agencies, policymakers and nongovernmental groups.
To inform the decisions and strategies of these stakeholders, The Economist Intelligence Unit and EIU Healthcare, its healthcare subsidiary, have conducted a study of the prevalence and costs of the top four modifiable risk factors that contribute to CVDs across the Asian markets of China, Australia, Hong Kong, Japan, Singapore, South Korea, Taiwan and Thailand.
Download the report to learn more.
The inroads of organised crime in the era of covid-19
Related content

Criminal asset recovery must become governments' central concern
This, in turn, has the effect of further polarising communities and alienating large segments of the population who already feel disenfranchised by an unequal distribution of global resources.
Are we sure there are no less destructive, more socially acceptable alternatives or, as a minimum, some ways to mitigate the impact of unpopular budgetary cuts?
It’s somehow striking that no political party is arguing that a significant contribution to the preservation of social cohesion should come from the recovery of the staggering amount of global wealth stolen through corruption, drug trafficking and other illicit trade that is currently nurturing rampant transnational criminal syndicates. When crime issues feature in electoral campaigns, it is usually to promise more police officers to patrol the streets and increased prison capacity, for example. But crime-control policies need not only represent a burden to state coffers. They can become a wealth-generating strategy if focused, determined and sustained efforts are made to recover stolen criminal assets, well beyond the currently half-hearted efforts.
Estimates by the UN Office on Drugs and Crime put the amount of money laundered globally in one year at 2-5% of global GDP, or US$2trn. To date, investments made in asset recovery efforts are a drop in the ocean. According to Europol, only 1.1% of criminal profits were confiscated in the EU between 2010 and 2014. If this figure were to increase by just a few percentage points, it could translate into a bonanza for national governments, potentially helping to avoid painful cuts to healthcare programmes, pensions for the elderly, subsidies for kindergartens and so on.
I often recall what former Cosa Nostra member Gaspare Mutolo declared in front of the Italian Anti-Mafia Parliamentary Committee back in 1993: “What bothers us most is when they take the money out of our pockets. One prefers to remain in jail with the money rather than being free without the money.”
So, why aren’t genuine, sustained and aggressive efforts being made to “follow the money” as a major path not only to deprive ever-expanding criminal networks of oxygen, but also to recover badly needed resources? After all, this is money that in one way or another has been syphoned from taxpayers’ pockets.
Let’s be fair. Following the money is akin to driving in a thick fog. Financial investigations are time and resource consuming, and fraught with obstacles. They often involve turning to foreign countries for help in tracing assets, freezing bank accounts held abroad and enforcing foreign confiscation orders. And while some authorities may be genuinely willing to assist, including through dedicated asset recovery offices, many are overstretched and not necessarily hoping for the phone to ring. Others are blatantly non-co-operative and pride themselves on their ability to shelter wealth (without asking too many questions about its origin) behind opaque regulations and corporate veils.
Even if investigators eventually succeed in having criminal assets traced, confiscated and turned over, they shouldn’t claim victory too quickly. The Italian experience is instructive. Currently, Italy is at the forefront of global efforts to confiscate criminal assets. Its legislative framework is one of the world’s most advanced and admired. And yet it is proving quite difficult to ensure that the approximately €30bn in assets seized and confiscated from Mafia organisations are effectively allocated for the purposes envisaged by the law: public and social re-use and, as a last resort, sale. Despite recent attempts to streamline procedures, Italy’s nine-year-old Agency for the Management and the Allocation of Seized and Confiscated Assets is still struggling with scarce resources and a Byzantine bureaucracy.
So, mission impossible? Not really. Many countries have already made criminal confiscations easier from a legal point of view, for example, by shifting from prosecutors to defendants the burden to prove that the assets in question are not derived from criminal conduct. Or by enabling authorities to broadly confiscate assets of criminal organisations without the need to establish a connection between those assets and specific criminal offences.
But above all, there seems to be momentum. The public at large, people from all walks of life and political affiliations, are increasingly frustrated at the sheer magnitude of organised crime, exposed by almost daily revelations of massive corruption and money-laundering schemes.
We need a new generation of aspiring politicians willing to invest time and political capital in championing criminal asset recovery as a central pillar of governments’ action. Initially, implementing such a strategy would require steep increases in the number of highly trained financial investigators, investments in big data analytics, and the allocation of significant resources to asset management and cross-border co-operation bodies. But in the medium term, these investments would yield a big payoff. Recovering even just an additional 5% of the globally stolen wealth could make a material difference to the daily lives of a large number of people who are struggling to make ends meet.
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the views of The Economist Intelligence Unit Limited (EIU) or any other member of The Economist Group. The Economist Group (including the EIU) cannot accept any responsibility or liability for reliance by any person on this article or any of the information, opinions or conclusions set out in the article.
The Global Illicit Trade Environment Index 2018
To measure how nations are addressing the issue of illicit trade, the Transnational Alliance to Combat Illicit Trade (TRACIT) has commissioned The Economist Intelligence Unit to produce the Global Illicit Trade Environment Index, which evaluates 84 economies around the world on their structural capability to protect against illicit trade. The global index expands upon an Asia-specific version originally created by The Economist Intelligence Unit in 2016 to score 17 economies in Asia.
View the Interactive Index >> Download workbook

Value-based healthcare in Sweden: Reaching the next level
The need to get better value from healthcare investment has never been more important as ageing populations and increasing numbers of people with multiple chronic conditions force governments to make limited financial resources go further.
These pressures, along with a greater focus on patient-centred care, have raised the profile of VBHC, especially in European healthcare systems. Sweden, with its highly comprehensive and egalitarian healthcare system, has been a leader in implementing VBHC from the beginning, a fact that was underscored in a 2016 global assessment of VBHC published by The Economist Intelligence Unit.
This paper looks at the ways in which Sweden has implemented VBHC, the areas in which it has faced obstacles and the lessons that it can teach other countries and health systems looking to improve the value of their own healthcare investments.
Suffering in silence: Assessing rare disease awareness and management in Asia-Pacific
As the region begins to get to grips with rare diseases, it will need to address significant challenges, some of which are still emerging. Health and social systems are making progress in many of these areas, but finding solutions remains a work in progress.
Related content

Video | Suffering in silence report highlights
Suffering in Silence: Assessing rare-diseases awareness and management in Asia-Pacific
Full reports:
Snapshots:
Australia | China | Japan | Korea | Taiwan
无声的苦难:中国大陆罕见病的认知与管理评估
日本における希少疾患の現状: 認知度・QoL向上に向けた課題と取り組み
침묵 속의 고통: 한국의 희귀질환 인 식 및 관리현황 평가
無聲的苦難:評估台灣對於罕見疾病之認知與管理
Video highlights:
English | Simplified Chinese | Japanese | Korean | Traditional Chinese

アジアにおける希少疾患: 認知度・QoL向上に向けた 課題と取り組み
そうした中で域内諸国は希少疾患がもたらす新旧様々な問題に直面している。医療・社会制度改革を通じた問題への対応が進んでいるものの、依然として効果的対策の模索が続く分野も多い。
ザ・エコノミスト・インテリジェンス・ユニット(EIU)がCSL ベーリングの協賛の下で作成した本報告書では、アジア太平洋地域5 カ国が希少疾患の分野で直面する課題と対応、診療体制の改革に向けた取り組みについて検証する。本報告書の作成に当たっては、医療関係者500名以上を対象としたアンケート調査、学術機関・医療機関・政府関係者・エキスパート患者16名に対する聞き取り調査、そして詳細にわたるデスクリサーチが実施された。
本報告書の作成にあたり、ザ・エコノミスト・インテリジェンス・ユニット(EIU)はアジア太平洋地域5 カ国の医療関係者503名を対象とするアンケート調査を2019 年11 〜12 月にかけて実施した。その目的は、希少疾患の認知レベルを理解し、各国政府が直面する課題を検証することだ。調査対象者の内訳は、専門医172 名、一般開業医229 名、看護師40 名、薬剤師62 名(いずれも現職)。国別の内訳は、オーストラリア103 名、中国100 名、日本100 名、韓国100 名、台湾100 名となっている。
また今回の調査では、医療者・患者団体関係者16 名を対象として、詳細にわたる聞き取り調査も実施した。ご協力をいただいた下記の皆様(アルファベット順に掲載・敬称略)には、この場を借りて御礼申し上げます:
国立研究開発法人 日本医療研究開発機構プログラムオフィサー 足立剛也 韓国国立生物医学医療センター希少疾患部門 Younjhin Ahn クイーンズランド工科大学eResearch 学部 ディレクターAPEC 希少疾患ネットワーク 議長Matthew Bellgard 西オーストラリア遺伝子検査サービスセンター未診断疾患プログラム担当ディレクターGareth Baynam 香港中文大学 準教授 Dong Dong シドニー大学小児科学・児童健康学担当教授Elizabeth Elliott 中国希少疾患協会 創立者 Kevin Huang アジア太平洋希少疾患連合理事長 Ritu Jain 千葉大学医学部附属病院脳神経内科 准教授 三澤園子 特定非営利活動法人 ASrid理事 西村由希子 台湾希少疾患基金共同創立者 Min-Chieh Tseng Rainbow Across Borders議長 Gregory Vijayendran Rare Cancers Australia理事長 Richard Vines 台中栄民総医院希少疾患・血友病センター ディレクターJiaan-Der Wang 疾病挑戦基金 事務局長 Yi'ou Wang 台湾健康増進部 事務次長 Chao-Chun Wu本調査プロジェクトはCSL ベーリングの協賛の下で実施された。報告書の執筆はPaul Kielstra、編集はEIU のJesse Quigley Jones が担当している。
Full reports:
Snapshots:
Australia | China | Japan | Korea | Taiwan
无声的苦难:中国大陆罕见病的认知与管理评估
日本における希少疾患の現状: 認知度・QoL向上に向けた課題と取り組み
침묵 속의 고통: 한국의 희귀질환 인 식 및 관리현황 평가
無聲的苦難:評估台灣對於罕見疾病之認知與管理
Video highlights:
English | Simplified Chinese | Japanese | Korean | Traditional Chinese

침묵 속의 고통: 아시아태평양 지 역내 희귀질환 인지도 및 질병관 리 현황 평가
희귀질환에 대한 이해와 함께 아태지역국가들은 중대한 과제들을 해결해야 하며 일부과제들은 아직도 부상 중이다. 많은 아태국가들의 보건사회제도가 발전하고 있지만해결책을 모색하는 과정은 아직도 진행 중이다
The Economist Intelligence Unit 의 이번보고서는 CSL Behring 의 후원으로 아태지역에서의 희귀질환의 양상을 살펴보고, 다섯아태 국가의 희귀질환 대응 수준 및 환자진료개선을 위한 정책들을 검토한다. 본 보고서는500 명 이상의 임상가, 16 명의 학계, 의료계, 정부, 환자 전문가들을 대상으로 한 설문조사와 광범위한 자료조사를 토대로작성되었다.
2019 년 11,12 월에 걸쳐 EIU 는 아시아태평양 지역에서의 희귀질환에 대한이해수준과 의료제도 차원의 과제를파악하기 위해 지역내 다섯 국가의 503 명의의료 전문가들을 대상으로 설문조사를실시했다. 설문 참가자들은 현직 전문의172 명, 일반의 229 명, 간호사 40 명, 약사62 명으로서, 국가별 분포는 호주 103 명,중국 100 명, 일본 100 명, 한국 100 명, 대만100 명과 같다.이와 더불어 16 명의 임상 전문가 및 환자단체 대표들과 자문/ 심층 인터뷰를 실시하였다. 지면을 빌어 아래의 전문가/대표들의 시간과 고견에 심심한 감사의 말씀을 전한다:
Takeya Adachi, 일본 의학연구개발소프로그램 담당 안윤진,한국 국립보건연구원생명의과학센터 난치성질환과 Matthew Bellgard, 호주 퀸즐랜드공과대학교 교수 및 전자연구소장, 아시아태평양경제협력체 (APEC) 희귀질환네트워크 의장 Gareth Baynam, 호주 웨스턴오스트레일리아 주 미진단 질환프로그램 유전학 서비스 과장 및 임상유전학 전문가 Dong Dong, 홍콩 특별자치구중문대학교 연구조교수 Elizabeth Elliott, 호주 시드니 대학교소아 청소년과 교수 Kevin Huang, 중국 희귀질환연합 창립자 Ritu Jain,싱가포르 아시아태평양 희귀질환연합 대표 Sonoko Misawa, 일본 지바대학교의과대학원 부교수 Yukiko Nishimura, NPO ASrid (일본희귀난치성 질환 이해관계자 권리증진서비스)창립 대표 Min-Chieh Tseng, 대만 희귀질환재단공동설립자 Gregory Vijayendran, Rainbow Across Borders대표 Richard Vines, 호주 Rare Cancers Australia 대표 Jiaan-Der Wang, 대만 타이충 보훈병원희귀질환 및 혈우병 센터장 Yi’ou Wang, Illness Challenge Foundation사무국장 Chao-Chun Wu, 대만 건강증진청 사무차장본 연구는CSL Behring사의 후원으로이루어졌으며 보고서 작성은 Paul Kielstra (EIU), 편집은 Jesse Quigley Jones(EIU)가 담당하였다.
Full reports:
Snapshots:
Australia | China | Japan | Korea | Taiwan
无声的苦难:中国大陆罕见病的认知与管理评估
日本における希少疾患の現状: 認知度・QoL向上に向けた課題と取り組み
침묵 속의 고통: 한국의 희귀질환 인 식 및 관리현황 평가
無聲的苦難:評估台灣對於罕見疾病之認知與管理
Video highlights:
English | Simplified Chinese | Japanese | Korean | Traditional Chinese
Covid-19: tracking the pandemic
17384
Related content

Covid-19: the greatest burden will fall on older people in low- and middle-...
We are living in unprecedented times. The covid-19 pandemic is escalating rapidly with more than 173, 300 confirmed cases and over 7,000 deaths in 152 countries and regions (see Figure 1). The majority of cases and deaths are among people aged 60 years and older living in low- and middle-income countries (LMICs) where healthcare resources to treat people and control the epidemic are limited.
Guidance largely ignores this issue in both high income countries (HICs) and LMICS, the latter of which contain 69% of the global population aged 60 years and over. Their health systems are also weaker, leaving them vulnerable to the worst impacts of covid-19. Limited guidance which is more relevant to HICs has been produced for older people but not for health and social care workers, care homes or day centres. No detailed age-specific data on global cases and mortality has been produced by the World Health Organisation (WHO) even though mortality rates jump sharply in older people, rising from 8% in those aged 70 to 79 years to 15% in those aged 80 and over (see Figure 2 which shows the effect of age on risk of dying from covid-19 from the Chinese outbreak).
In the absence of clear comprehensive guidelines for prevention and control of covid-19 among older people, ad hoc policies are emerging. In Italy scarce hospital and intensive care services are being prioritised for younger, otherwise healthy patients over older patients, according to reports. In the UK, people aged 70 and over will be expected to self-isolate themselves for up to four months in the coming weeks.
In LMICs, older people provide an integral economic and social resource to societies, including bringing up grandchildren to support the labour mobility of their adult children and relatives. Beyond grief and bereavement the implications of covid-19 deaths among the older population will be profound, especially when family members working abroad are unable to return home at short notice.
Increasing numbers of very old people are now being cared for in nursing homes in LMICs. These homes are often unregulated, provide care of very poor quality and may even act as incubators of infection (as do cruise ships, prisons, mines and HIC nursing homes). Outbreaks in LMIC institutions would have serious implications, further underpinning the need for international guidance similar to that issued recently by the International Federation of the Red Cross and Red Crescent Societies, UNICEF and the WHO regarding children and schools.
The ability of health systems to cope with a surge in demand is extremely limited, especially for patients needing intensive care. Health systems in LMICs face severe constraints on capacity at normal times and are unlikely to be able to keep up, especially if the precarious staffing levels—already depleted by migration, low salaries and poor working conditions—and limited gerontological expertise are reduced further by illness. The needs of older people are not being adequately addressed in developing covid-19 policy and practice. Current social distancing policies ignore the precarious existence of many older people and fail to account for the realities faced by those living alone and individuals who are dependent on others. The high levels of illiteracy in LMICs also present a challenge which has yet to be considered in any meaningful way.
An age perspective needs to be explicitly included in the development of national and global planning for covid-19, and it is increasingly clear that a global expert group should be formed to provide support and guidance for older people, home carers, residential facilities and overburdened hospitals in LMICs.
Shah Ebrahim is an honorary professor of public health at the London School of Hygeine & Tropical Medicine. He would like to thank Peter Lloyd- Sherlock, professor of social policy and international development, University of East Anglia; Leon Geffen, Samson Institute for Ageing Research, Cape Town, South Africa; and Martin McKee, professor of European public health, London School of Hygiene & Tropical Medicine, for contributing to this article. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the views of The Economist Group or any of its affiliates. The Economist Group cannot accept any responsibility or liability for reliance by any person on this article or any of the information, opinions or conclusions set out in the article.

The secret life of coronavirus: Why we need such drastic social distancing...
Left unchecked, the novel coronavirus (covid-19) will continue to sweep the globe. The horror stories from emergency departments and initial estimates of fatality rates starkly portend large numbers of people dying from both the virus and insufficient healthcare capacity. However, there is disagreement about what it will take to halt this progression and how far our preventative measures should go.
Our analysis in early February of 458 confirmed covid-19 cases across 93 Chinese cities was one of the clear early warnings that without interventions the average time between successive cases in a transmission chain is less than a week (around four days). Moreover, people can spread covid-19 before they even know they are sick, and there are individuals known as “super-spreaders” who infect an unusually large number of others.
These data help us understand why covid-19 is measurably more difficult to contain than a similar virus, SARS (severe acute respiratory syndrome). It comes down to a race between humans and the virus—how rapidly we can track down an infected person’s contacts versus how quickly the viral infection can incubate and spread.
While covid-19 moves quickly and sometimes silently, SARS is slow and visible. The serial interval of each demonstrates why covid-19 is the more insidious threat: if person A infects person B, the serial interval is the time between person A developing symptoms and person B developing symptoms. SARS has a serial interval of around eight days—twice as long as covid-19—and no pre-symptomatic transmission.
Imagine that a patient is diagnosed with SARS two days after first feeling sick. Public health authorities would have time on their side, perhaps a full six days to track down and isolate anyone who had contact with the patient over the prior two days. With covid-19, by the time of diagnosis a patient may have already been contagious for several days. During this period they may have infected many others who are also now spreading the virus—possibly without displaying any symptoms.
This is why covid-19 requires more drastic measures than SARS. It can spread quickly and silently, and we cannot possibly identify every infectious individual in an emerging outbreak, particularly with limited laboratory-testing capacity.
Super-spreading events compound the challenge. Among the 458 Chinese cases, five people infected over five others, with the biggest super-spreader infecting at least 16 people. Network theory—the mathematics that underlies the computer models that predict how the disease will spread— tells us that even a few people capable of infecting large numbers of others can dramatically amplify transmission and undermine interventions.
The recent threats of SARS, swine flu, Ebola, and Zika have brought fame to an epidemiological statistic known as R0. It stands for the basic reproduction number and is intended to be an indicator of the contagiousness of infectious agents (it is pronounced R-naught). In short it tells us how many people each new case will infect during the early days of a pandemic on average. An outbreak is expected to continue if R0 has a value >1 and to end if R0 is <1.
A lot of attention has been paid to recent estimates suggesting that covid-19 has a lower R0 than SARS, roughly two versus three. Clearly, then, R0 is not the whole story. It indicates whether one case will turn into two or three or four, but not how quickly or how silently that will come to pass.
The level of intervention required to curb an outbreak very much depends on all three factors: its R0 value, speed, and visibility in the community. We should not be fooled by the relatively modest R0 of covid-19 as its speed and stealth make it all the more difficult to contain. Even if each case infects only two others, the number of infections can skyrocket undetected in the absence of early and extensive control measures that limit person-to-person contact.
Our study highlights the elusiveness of covid-19. Keeping people apart is the only guaranteed way to block infections given the immense challenge of identifying contagious and soon-to-be contagious cases. Whether the policy goal is to stop transmission, protect those at high risk, or "flatten the curve" to ensure that fewer people are sick at any one time, extreme social distancing strategies of the type we have been seeing are strongly recommended.
Professor Lauren Ancel Meyers is the Cooley Centennial Professor of biology and statistics at the University of Texas at Austin, where she develops powerful mathematical methods for forecasting the spread of diseases and designing effective disease control strategies. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the views of The Economist Group or any of its affiliates. The Economist Group cannot accept any responsibility or liability for reliance by any person on this article or any of the information, opinions or conclusions set out in the article.

Covid-19 pandemic accelerates the rise of digital payments
China, South Korea and the US Federal Reserve have started quarantining or disinfecting banknotes. It is well-known that currency in circulation can serve as a vehicle for transmitting pathogens, though the potency of pathogens transmitted via cash remains unclear. The human influenza virus, for example, can remain alive and infectious for more than two weeks on banknotes. Although it’s not known whether the exchange of currency infected with influenza can dramatically increase its spread, responses from the US, Korean and Chinese governments raise concerns.
It’s possible that these governments are simply taking extreme precautionary measures. It’s also possible that physical currency can indeed be a significant transmission medium for highly infectious diseases such as covid-19. A local branch of the People's Bank of China in Guangzhou has even opted to destroy banknotes that have been in circulation in high-risk settings such as hospitals or wet-markets.
These measures reflect earlier governmental responses to infectious disease. A late 1940s report on Egypt’s cholera epidemic highlighted the viability of cholera pathogens on banknotes. Throughout history people have responded to sickness in a similar way by washing or fumigating banknotes, yet we still have limited understanding of how physical currencies might transmit new pathogens.
There’s no doubt that covid-19 will accelerate the pre-existing trend towards digital payments in Asia, and China in particular. In late October 2019, Chinese President Xi Jinping endorsed blockchain—a digital ledger technology on which digital currencies can be transacted—as “an important breakthrough for independent innovation of core technologies”. He added that the People’s Bank of China intended to replace cash with a government-issued digital currency. The Chinese government actively promotes its internet banking infrastructure, whereas Western nations rarely use a top-down approach to governance.
In China, where digital payments are already prevalent, covid-19 could be a significant driver for the total elimination of cash. In 2018, nearly 73% of Chinese internet users made online payments (up from 18% in 2008). According to a recent survey by Deutsche Bank, this increase is partly driven by young people who are typically more open to adopting new technologies. China and Southeast Asian countries have much larger young populations than Europe and the US.
Western countries have tended to move at a slower pace towards digital payments than, for example, China. Part of the reason for this lies, according to Deutsche Bank, in different payment cultures of countries. A third of the people in OECD countries consider cash to be their favourite payment method, and more than half believe cash will always be around. Citizens in many European countries (notably Germany) and those in the US have a marked preference for cash.
Source: Deutsche Bank, The Future of Payments.
But even in Western countries that share similar payment cultures we can observe variation in digital preparedness. In terms of homegrown fintech champions that could benefit most from a digital payments transition, Europe’s are much smaller in size than large US counterparts such as Apple Pay, Google Pay, and PayPal—to name a few. Beyond that, many of Europe’s leading digital payment service companies are controlled or backed by US and Chinese companies (eg Swedish financial technology company IZettle was recently acquired by PayPal and Germany’s mobile N26 bank is backed by China’s Tencent).
Nonetheless, European countries are determined to be at the forefront of digital currencies. Central banks such as the Bank of England, the European Central Bank, the Swiss National Bank and the Swedish Riksbank have started to assess the feasibility of digital central bank currencies. These would perform all the functions of banknotes and coins and could then be used by households and businesses to make both payments and savings. The transition will not be easy. Digital central bank currencies require infrastructure that can record in-person and online transactions, which means that governments will need private sector co-operation.
Under “normal” conditions it would take a long time to change culturally ingrained habits and institutional legacies related to long and well-established payments systems. Jodie Kelley—CEO of the US Electronic Transactions Association—said in a recent interview that “people default to what’s familiar, unless there’s something to jolt you out of it”. She continued that “contactless payments have come up as a new option for consumers who are much more conscious of what they touch”.
The covid-19 pandemic could move the world more rapidly towards digital payments. In France, the Louvre museum in Paris recently banned cash due to covid-19 fears. The museum did this even though its policy clashes with the Bank of France's requirement that all businesses accept cash.
It is too early to conclude what the changes might look like in each cultural, demographic, and institutional context, but we can be sure that covid-19 is already reinforcing existing trends towards increased digitisation of payments.
Dr Marion Laboure and Sachin Silva are the co-authors of this blog. Marion Laboure is a macro strategist at Deutsche Bank and Sachin Silva is a doctoral candidate and fellow at Harvard University specialising in global health and economics.
The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the views of The Economist Group or any of its affiliates. The Economist Group cannot accept any responsibility or liability for reliance by any person on this article or any of the information, opinions or conclusions set out in the article.
The secret life of coronavirus: Why we need such drastic social distancing measures
Related content

Value-based healthcare in Sweden: Reaching the next level
The need to get better value from healthcare investment has never been more important as ageing populations and increasing numbers of people with multiple chronic conditions force governments to make limited financial resources go further.
These pressures, along with a greater focus on patient-centred care, have raised the profile of VBHC, especially in European healthcare systems. Sweden, with its highly comprehensive and egalitarian healthcare system, has been a leader in implementing VBHC from the beginning, a fact that was underscored in a 2016 global assessment of VBHC published by The Economist Intelligence Unit.
This paper looks at the ways in which Sweden has implemented VBHC, the areas in which it has faced obstacles and the lessons that it can teach other countries and health systems looking to improve the value of their own healthcare investments.

Breast cancer patients and survivors in the Asia-Pacific workforce
With more older women also working, how will the rising trend of breast cancer survivorship manifest in workplace policies, practices and culture? What challenges do breast cancer survivors face when trying to reintegrate into the workforce, or to continue working during treatment? How can governments, companies and society at large play a constructive role?
This series of reports looks at the situation for breast cancer survivors in Australia, New Zealand and South Korea. It finds that while progress has been made, more needs to be done, particularly in South Korea, where public stigma around cancer remains high.
The Cost of Silence
Cardiovascular diseases levy a substantial financial toll on individuals, their households and the public finances. These include the costs of hospital treatment, long-term disease management and recurring incidence of heart attacks and stroke. They also include the costs of functional impairment and knock-on costs as families may lose breadwinners or have to withdraw other family members from the workforce to care for a CVD patient. Governments also lose tax revenue due to early retirement and mortality, and can be forced to reallocate public finances from other budgets to maintain an accessible healthcare system in the face of rising costs.
As such, there is a need for more awareness of the ways in which people should actively work to reduce their CVD risk. There is also a need for more primary and secondary preventative support from health agencies, policymakers and nongovernmental groups.
To inform the decisions and strategies of these stakeholders, The Economist Intelligence Unit and EIU Healthcare, its healthcare subsidiary, have conducted a study of the prevalence and costs of the top four modifiable risk factors that contribute to CVDs across the Asian markets of China, Australia, Hong Kong, Japan, Singapore, South Korea, Taiwan and Thailand.
Download the report to learn more.
Covid-19 pandemic accelerates the rise of digital payments
Related content

Covid-19: the greatest burden will fall on older people in low- and middle-...
We are living in unprecedented times. The covid-19 pandemic is escalating rapidly with more than 173, 300 confirmed cases and over 7,000 deaths in 152 countries and regions (see Figure 1). The majority of cases and deaths are among people aged 60 years and older living in low- and middle-income countries (LMICs) where healthcare resources to treat people and control the epidemic are limited.
Guidance largely ignores this issue in both high income countries (HICs) and LMICS, the latter of which contain 69% of the global population aged 60 years and over. Their health systems are also weaker, leaving them vulnerable to the worst impacts of covid-19. Limited guidance which is more relevant to HICs has been produced for older people but not for health and social care workers, care homes or day centres. No detailed age-specific data on global cases and mortality has been produced by the World Health Organisation (WHO) even though mortality rates jump sharply in older people, rising from 8% in those aged 70 to 79 years to 15% in those aged 80 and over (see Figure 2 which shows the effect of age on risk of dying from covid-19 from the Chinese outbreak).
In the absence of clear comprehensive guidelines for prevention and control of covid-19 among older people, ad hoc policies are emerging. In Italy scarce hospital and intensive care services are being prioritised for younger, otherwise healthy patients over older patients, according to reports. In the UK, people aged 70 and over will be expected to self-isolate themselves for up to four months in the coming weeks.
In LMICs, older people provide an integral economic and social resource to societies, including bringing up grandchildren to support the labour mobility of their adult children and relatives. Beyond grief and bereavement the implications of covid-19 deaths among the older population will be profound, especially when family members working abroad are unable to return home at short notice.
Increasing numbers of very old people are now being cared for in nursing homes in LMICs. These homes are often unregulated, provide care of very poor quality and may even act as incubators of infection (as do cruise ships, prisons, mines and HIC nursing homes). Outbreaks in LMIC institutions would have serious implications, further underpinning the need for international guidance similar to that issued recently by the International Federation of the Red Cross and Red Crescent Societies, UNICEF and the WHO regarding children and schools.
The ability of health systems to cope with a surge in demand is extremely limited, especially for patients needing intensive care. Health systems in LMICs face severe constraints on capacity at normal times and are unlikely to be able to keep up, especially if the precarious staffing levels—already depleted by migration, low salaries and poor working conditions—and limited gerontological expertise are reduced further by illness. The needs of older people are not being adequately addressed in developing covid-19 policy and practice. Current social distancing policies ignore the precarious existence of many older people and fail to account for the realities faced by those living alone and individuals who are dependent on others. The high levels of illiteracy in LMICs also present a challenge which has yet to be considered in any meaningful way.
An age perspective needs to be explicitly included in the development of national and global planning for covid-19, and it is increasingly clear that a global expert group should be formed to provide support and guidance for older people, home carers, residential facilities and overburdened hospitals in LMICs.
Shah Ebrahim is an honorary professor of public health at the London School of Hygeine & Tropical Medicine. He would like to thank Peter Lloyd- Sherlock, professor of social policy and international development, University of East Anglia; Leon Geffen, Samson Institute for Ageing Research, Cape Town, South Africa; and Martin McKee, professor of European public health, London School of Hygiene & Tropical Medicine, for contributing to this article. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the views of The Economist Group or any of its affiliates. The Economist Group cannot accept any responsibility or liability for reliance by any person on this article or any of the information, opinions or conclusions set out in the article.

Beyond Cash: China’s Emerging Payments Market
As China’s economy continues its robust expansion, and as its banking sector finally opens up to foreign competition, the demand for credit is taking off. Local banks have ramped up their operations for the last three or four years in preparation for increased competition from foreign rivals. As their efforts bear fruit, the potential for China’s payment cards market has never looked better.
Nowhere is this more so than in China’s emerging market for debit and credit cards. With more than 200m new cards issued last year alone, China’s total number of plastic cards broke though the one billion mark in 2006, with no sign of the pace abating. While a relatively tiny portion of this total—some 50 million—are currently credit cards, growth rates for the sector (both in terms of spending and transaction volumes) are now much higher than for the mass-market debit cards that form the bulk of cards in circulation. No surprise, then, that foreign banks are now eyeing this space for opportunity.
The main findings of our research are as follows:
Retail banks are very bullish on consumer banking in general—and credit cards in particular... For many of the retail banks surveyed for this report, credit cards are the main priority. When asked what products they believe hold the greatest prospects for China’s personal banking industry, retail bankers were most optimistic about credit cards and bank accounts. Fifty-fivepercent of study respondents believe the prospects for these consumer banking products are ‘highly promising’ over the next three years. Debit cards are seen as the next most promising item (45%), although these are directly linked to the prospects for basic bank accounts, followed by wealth and investment management (40%). In fact, respondents report overwhelmingly positive views for all aspects of the consumer banking sector. ...But the outlook for profits is less certain. When it comes to profits in the credit card market, our survey respondents are less confident. Forty-three percent agree that it would be difficult to make a profit in the credit card market over the next three years, compared with 36% who remain uncertain and just 21% who believe it is possible. The key issue is tough competition for customers between local banks growing their market share and foreign rivals trying to establish a beach head in China. This competition inevitably leads to lower card fees, which keeps earnings low (or negative). In addition, banks are grappling with low rates of revolving credit on cards, resulting from a cultural aversion to accruing debt, together with low fees and interest rates that issuers are allowed to levy on merchants and card users. Infrastructure is key to growth in the cards market. According to the executives surveyed for this report, improving infrastructure – encompassing both merchants and ATMs—will play the biggest role in encouraging the increased acceptance of card payments in China. Fully 83% of retail bankers polled chose this as an essential requirement. This component scores far ahead of any other criteria, for example better collaboration between key stakeholders such as banks and payment processors (48%) or publicity campaigns (33%). When asked what the Chinese market needs to supporta payments infrastructure, half of the survey respondents selected better availability of consumer credit-history data. Merchant acquisition is a major hurdle. Convincing merchants to accept credit cards is a major challenge for banks. Eight out of ten retail bankers polled for this report say that local retailers’ preference for cash is either a ‘very significant’ or ‘significant’ barrier in operating cards and payment services. In part, this is because retailers don’t yet feel much pressure from customers to provide payment card facilities in a society where cash is traditionally preferred. Despite an opening financial market, much risk remains. More than half (53%) of bankers polled for this report selected political risk, relating to policy and regulation, as the biggest existing or potential risk associated with their firm’soperations in China. Retail bankers in particular listed licensing risk (chosen by 43%) as a major concern, second only to political risk, highlighting the difficulties associated with getting permission to expand into new regions or markets. Along with this, 41% of the respondents expressed a general concern about the outlook for China’s banking industry.Much work needs to be done to promote a plastic card payment culture in China. More than anything else, a more extensive card network and infrastructure must be rolled out to promote consumer usage. Along with this, databases of consumers’ credit and transaction histories require expansion. In addition, Chinese consumers must be encouraged to make the switch from cash-based transactions to plastic cards. Despite these challenges, growth is already strong. And in cities such as Beijing, efforts to prepare for the 2008 Summer Olympic Games will help create an environment that supports card payments. Although foreign banks entering the market will have their work cut out, the opportunity is simply too big to ignore.

Value-based healthcare in Sweden: Reaching the next level
The need to get better value from healthcare investment has never been more important as ageing populations and increasing numbers of people with multiple chronic conditions force governments to make limited financial resources go further.
These pressures, along with a greater focus on patient-centred care, have raised the profile of VBHC, especially in European healthcare systems. Sweden, with its highly comprehensive and egalitarian healthcare system, has been a leader in implementing VBHC from the beginning, a fact that was underscored in a 2016 global assessment of VBHC published by The Economist Intelligence Unit.
This paper looks at the ways in which Sweden has implemented VBHC, the areas in which it has faced obstacles and the lessons that it can teach other countries and health systems looking to improve the value of their own healthcare investments.
Covid-19: the greatest burden will fall on older people in low- and middle-income countries
Related content

Value-based healthcare in Sweden: Reaching the next level
The need to get better value from healthcare investment has never been more important as ageing populations and increasing numbers of people with multiple chronic conditions force governments to make limited financial resources go further.
These pressures, along with a greater focus on patient-centred care, have raised the profile of VBHC, especially in European healthcare systems. Sweden, with its highly comprehensive and egalitarian healthcare system, has been a leader in implementing VBHC from the beginning, a fact that was underscored in a 2016 global assessment of VBHC published by The Economist Intelligence Unit.
This paper looks at the ways in which Sweden has implemented VBHC, the areas in which it has faced obstacles and the lessons that it can teach other countries and health systems looking to improve the value of their own healthcare investments.

Breast cancer patients and survivors in the Asia-Pacific workforce
With more older women also working, how will the rising trend of breast cancer survivorship manifest in workplace policies, practices and culture? What challenges do breast cancer survivors face when trying to reintegrate into the workforce, or to continue working during treatment? How can governments, companies and society at large play a constructive role?
This series of reports looks at the situation for breast cancer survivors in Australia, New Zealand and South Korea. It finds that while progress has been made, more needs to be done, particularly in South Korea, where public stigma around cancer remains high.
The Cost of Silence
Cardiovascular diseases levy a substantial financial toll on individuals, their households and the public finances. These include the costs of hospital treatment, long-term disease management and recurring incidence of heart attacks and stroke. They also include the costs of functional impairment and knock-on costs as families may lose breadwinners or have to withdraw other family members from the workforce to care for a CVD patient. Governments also lose tax revenue due to early retirement and mortality, and can be forced to reallocate public finances from other budgets to maintain an accessible healthcare system in the face of rising costs.
As such, there is a need for more awareness of the ways in which people should actively work to reduce their CVD risk. There is also a need for more primary and secondary preventative support from health agencies, policymakers and nongovernmental groups.
To inform the decisions and strategies of these stakeholders, The Economist Intelligence Unit and EIU Healthcare, its healthcare subsidiary, have conducted a study of the prevalence and costs of the top four modifiable risk factors that contribute to CVDs across the Asian markets of China, Australia, Hong Kong, Japan, Singapore, South Korea, Taiwan and Thailand.
Download the report to learn more.