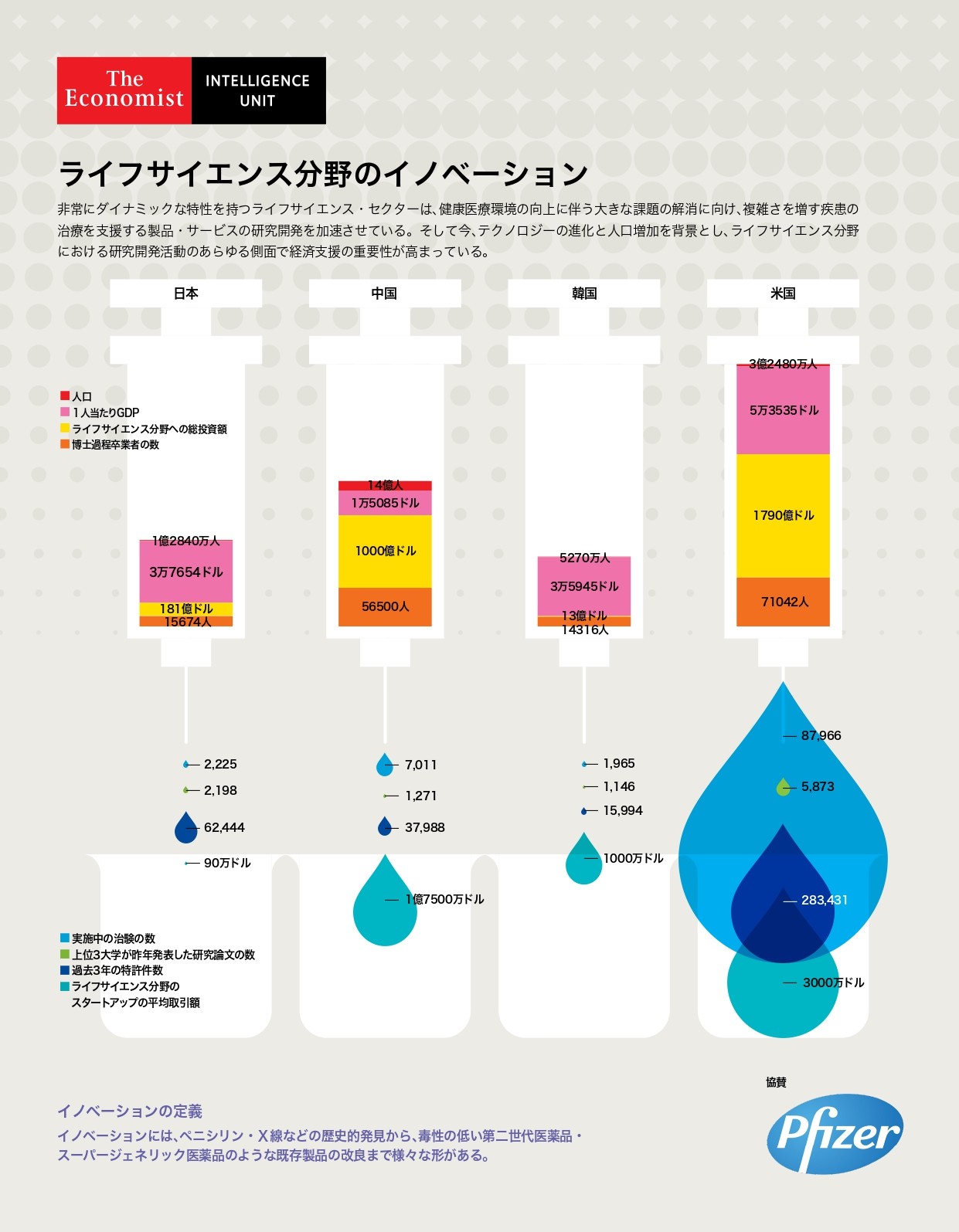
ライフサイエンス分野のイノベーション- インフォグラフィック
Download InfographicHealth
ライフサイエンス分野のイノベーション- インフォグラフィック

Jesse is a managing editor for Economist Impact based in Asia, with a focus on healthcare.
Based in Hong Kong, Jesse has been working in Asia for over 10 years. Prior to the Economist Impact, he held roles in medical education, scientific publications and medical communications, working in multinational biopharmaceutical companies with a focus in vaccines and biologic medicines. Jesse has extensive experience researching and collating medical information and working with healthcare professionals and patient organisations to develop insight-driven communications programmes.
Jesse holds a BSc in Anatomy and Physiology from the University of Leeds. His editorial interests include the policy response to emerging public health issues and patient advocacy in infectious diseases.
More from this series
Related content

持続可能な医療の実現に向け: 新たな構造改革のビジョン
過去60年、日本は比較的小規模な制度改革により、優れた医療サービスを提供している。国民皆保険制度を通じ、手ごろな価格で最先端の医療サービスを受けられる、つまり高いレベルのユニバーサル・ヘルス・カバレッジ(UHC)を実現してきた。
日本の医療制度の適用範囲が非常に広いために、政策立案者らによる痛みを伴う改革の先延ばしを招いた面もある。先進医療の高額化が進む現在、需給バランス調整メカニズムの欠如、人口の高齢化がもたらす負荷、医療経済性の検討といった大きな課題が浮上している。こうした現状は医療制度、ひいては社会・経済全体の持続可能性に大きな影響を及ぼす可能性が高い。
日本が医療保険制度におけるインセンティブ強化を今進めなければ、先進イノベーションの活用や質の高いUHCの維持が困難になる恐れがある。ザ・エコノミスト・インテリジェンス・ユニット(EIU)が今回作成したスコアカードの結果も、抜本的改革の必要性を示唆している。
日本の医療には、治療費が高額で医療格差の目立つ米国と比較すれば優れた面が多い。しかし制度的な持続可能性を左右する5つの要因のうち4つで英国・フランスに大きな差をつけられており、韓国にも後れを取っているのが現状だ。
特に包括医療・研究開発制度の領域では取り組みの遅れが目立ち、適切な人員体制や説明責任のレベル、患者中心の医療の推進といった面でも改善の余地は大きい。ただし、長期ケア体制の確立については高い評価を獲得している。今回の調査で明らかとなった主要な論点は次ページの通り。
主要な論点:
医療財政の持続可能性は急速に低下しつつある 現行の診療報酬制度は抜本的構造改革の足かせとなっている 医療資源の効率的活用に向けたインセンティブの見直しが求められている 日本の長期ケア制度は世界的にも優れているが、プライマリケアとの連携強化は大きな課題 日本の研究開発体制は他の先進国に後れを取っている
Health system sustainability in Japan: Priorities for structural reform
Japan’s healthcare system has kept the country remarkably healthy with relatively minor changes for nearly six decades. The system provides universal care, generous coverage and the most innovative treatments at a cost that is accessible to all.
Yet the very scope of coverage in the Japanese system obscures the extent to which policymakers have put off making necessary but difficult choices. In particular, the lack of regulation of demand for health services, the pressures of an ageing population and the underdeveloped system for evaluating efficiency and effectiveness of medical products and services could paralyse Japan’s healthcare system as the cost of state-of-the-art medical treatments increase. The economic consequences of this would inevitably reverberate beyond the health system itself.
Without changes in the incentives built into the current system, Japan will struggle to take advantage of medical innovation and to maintain its ability to deliver high-quality, accessible care in the future. As our Health system sustainability in Japan scorecard shows, there are signs that significant fixes to the system may be necessary. Although Japan compares well in many respects to the more expensive and fragmented system in the US, it lags significantly behind the UK and France, and slightly behind neighbouring South Korea, in four of the five principal scoring domains.
Japan’s health system compares especially unfavourably with regard to progress in integrated healthcare and research preparedness, but it also has ground to make up in adequate workforce staffing and in the accountability and patient-centredness of the system. At the same time, it scores well in the provision of a long-term care network. We highlight the report’s key findings below.
Key findings:
Japan’s health financing system is becoming increasingly unsustainable. The country’s existing price review process acts as a brake on structural health system reform. Different incentives are needed to efficiently use medical workforce and hospital resources. Japan’s long-term care system can be a model for other countries but needs better integration with primary care. Japan lags behind developed country peers in the area of research.Download the report to find out more.