The Gulf states have an obesity problem. Between 31% and 43% of people in each of the six Gulf Cooperation Council (GCC) nations are obese, a proportion that grows to almost three-quarters when including overweight people.
As with the other GCC countries, Kuwait has seen rapid development in recent decades. Since the end of the Gulf War in 1991, GDP has increased more than tenfold, in step with industrialisation, urbanisation and rapid population growth. Among changes in the social and cultural environment, physical activity has declined and diets have deteriorated, driven by a proliferation of fast-food chains and dining-out culture, and the availability of relatively cheap fatty and sugary foods. Obesity is epidemic, yielding direct and indirect healthcare costs of US$2.8bn annually.
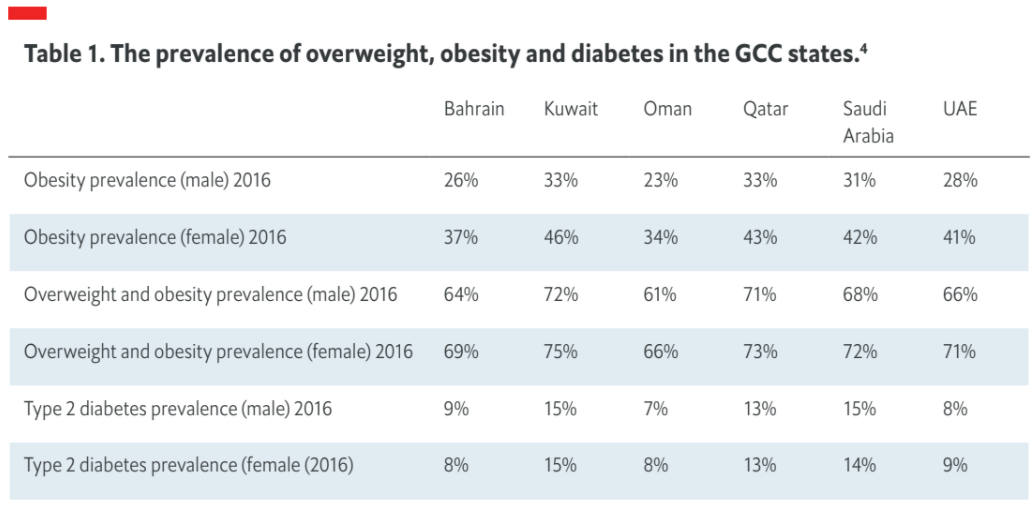
The increase in obesity and overweight in the past two decades covers all demographics. However, the prevalence of obesity is more pronounced among women (about 46% in 2016, versus about 33% in men), who have limited access to sports and exercise, and who tend to spend more time at home, engaged in sedentary behaviour. Children and young people are also disproportionately affected, a factor that is especially significant in a region where over half of the population is younger than 25. One study found that as many as 30% of secondary-school children in Kuwait are obese. The relatively young populace means that population-level impacts will be increasingly pronounced as current generations of children grow older.
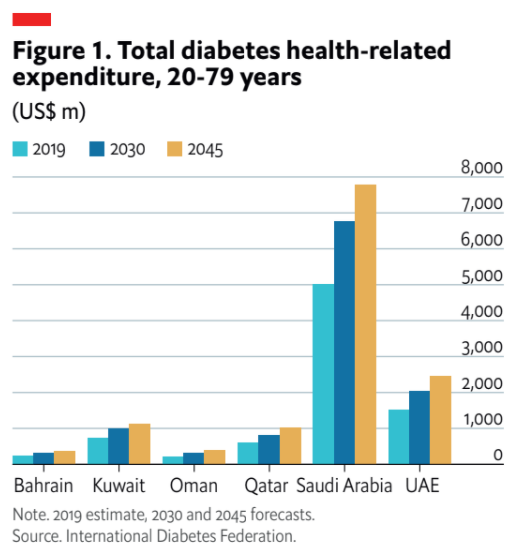
One prevalent consequence of obesity in Kuwait is diabetes (not all diabetes patients are obese, but about 90% are, and people who are obese are five times more likely to have type 2 diabetes). According to the International Diabetes Federation, diabetes prevalence among adults in Kuwait is 22%, more than double the global average. The disease is also more prevalent among every age group than it is anywhere else in the world—including among 64.8% of over 60s (more than three times the global average for this age group) and 5.4% of 20-29-year-olds.10 There is also a direct economic cost: currently, Kuwait spends over US$1,000 per diabetes patient, and the cost to health services is expected to grow as the population ages.
Plans and prevention needed
Policymaking to manage the obesity epidemic has lagged behind that of other regions, although GCC nations are increasingly looking to implement new initiatives. For example, a tax on sugary foods has gradually been brought in by GCC countries in recent years; Kuwait was the last of the six nations to do so, in 2020, when it saw a year-on-year reduction in growth rates of soft drink sales from 6.3% to 5.5%.
In terms of national plans, all GCC countries have developed documents on health promotion, but these tend to be limited in terms of tangible goals, follow-up and specific procedures. In addition, implementation and follow-up of such plans often does not take place, and health promoters and educators are rarely involved in their development. In general, intersectoral involvement is low in Kuwait, when the collaboration of schools, various government ministries, the media and the pharmaceutical industry should be a key part of the strategy.
“There is some co-operation between the health and education ministries, but it is not up to level in my personal opinion, and mass media is probably under-used in the education of the public,” says Yousef Bo-Abbas, founder of the Kuwait Obesity Association and a consultant of endocrinology at the Ministry of Health.
In addition, the WHO has highlighted a lack of adequate communication between health facilities and programmes operated by the Ministry of Health. (Kuwait’s health system is divided into six decentralised sub-regions, each of which have significant autonomy.) The WHO also highlights what it describes as an “underdeveloped health promotion programme” in Kuwait—including inadequate school- and workplace-focused and food- labelling measures, and lays out specific necessary in relation to NCDs.
Dr Bo-Abbas says that efforts to create standard GCC policies on obesity prevention have stalled amid the COVID-19 pandemic. He adds that although individual country plans are “great on paper”, their implementation is “really not up to standard”. Furthermore, he says that conflicting interests pose a significant challenge: “We need drastic measures that would interfere with the best interests of the fast-food companies and sugar and oil companies that have so much political power.”
Moving beyond surgery
The chronic nature of the Gulf’s obesity problem has been reflected by a significant embrace of bariatric surgery in the region. In Kuwait, the rate of bariatric operations is the highest in the world as a percentage of the population (0.16%), almost twice as high as in the second-placed country, Sweden, and about 15 times the global average. Dr Bo-Abbas says that an “easy-fix approach” is behind the high rates of surgery, adding that “patients think that surgery is the easiest and fastest” solution. However, although the benefits of bariatric surgery are clear for more severe cases, there are also risks, and surgery will not be suitable (or desirable) for everyone.
An increasingly important alternative to surgery is nutrition-focused lifestyle interventions. Such treatment, which relies on modest, incentivised weight loss, tends to be based on three main elements: decreased calorific intake and a more nutritious diet, increased physical activity, and behavioural support and education. Medication is also likely to be an element of treatment, especially for patients with diabetes.
These interventions are best administered by a multidisciplinary team (MDT), consisting of a primary physician, nurse (or nurse practitioner), dietitian, exercise physiologist, behaviourist and, in some cases, a pharmacist. In addition to the range of expertise offered in the MDT model (which spans lifestyle-based and surgical interventions, and allows for a relatively smooth transition between the two), often, given the dovetailing nature of the two conditions, diabetes and obesity MDTs will share personnel, offering a more integrated overall service.
Incentivising a person to change their diet and physical activity is a difficult process. Most obviously, it involves significant habitual change, which is especially difficult when unhealthy eating and sedentary behaviour are ingrained features of someone’s life. The shift to maintained lower calorific intake is reliant on education in terms of both nutrition and meal planning and preparation. This can take time, potentially making behavioural interventions difficult to adopt, even when meal plans are employed, as they often are.
Supplementing a healthy diet
One way of easing adherence to reduced- calorie diets is by replacing certain meals with a dietary supplement, often in the form of a shake. Such supplements are nutritionally balanced to reduce intake of fats and carbohydrates and increase levels of fibre and protein, thereby increasing metabolism and reducing the ratio of fat to so-called lean mass—muscle, essentially.
There is evidence of the success of such approaches. Why WAIT, a programme run by a hospital in the US city of Boston, incorporated nutritional supplement shakes as part of a low glycaemic index, high-fibre diet, reducing calorific intake in most participants by 500 calories. A range of benefits were seen in patients with type 2 diabetes. For example, weight loss was significant, at an average of 8.3kg (11.9% weight loss) after a year. Levels of haemoglobin A (HbA1c), which is elevated in those with diabetes, decreased to the target level among 82.3% of patients. A follow-up study found that HbA1c levels continued to improve for five years after the start of the intervention, while blood pressure reduced continually over the first 18 months.
Another study found that a similar diet, which included nutritional meal replacement shakes at breakfast and as an afternoon snack, improved post-prandial glycaemic response, night-time glucose variability and cravings for starchy foods. Another found that a structured, calorie-controlled diet facilitated weight loss when initiated a year after patients had undergone gastric bypass surgery.
Diet is one part of a broad cultural shift
Non-compliance to healthy diets is one of the biggest barriers to their success—changing ingrained habits is difficult. Bariatric surgery is likely to be a better option than lifestyle-based interventions for many people, but the opposite will be equally true for many others; even among those undergoing surgery, a healthier diet is important in the longer term. For less severe cases of overweight, improved diet and nutrition is clearly going to be preferable as a less-invasive option than surgery, even if as the initial part of a stepped- care model managed by an obesity or diabetes MDT.
Overall, though, more must be done to improve the health—and health knowledge— of the population in Kuwait and the GCC, from prevention to treatment. That Kuwait is a wealthy country with a modern health system that collects a vast amount of data suggests that it has the ability to effectively promote the uptake of healthy behaviours within the country while offering medical care as required. However, broad-based progress is needed. Doing so will involve collaboration between various government bodies—notably the health and education ministries—along with academia and the media.




