-
Stakeholders from the five countries, focused in this report, highlighted a lack of awareness of AFib and its consequences as one of the most significant challenges for the condition. The lack of awareness manifests in different ways and among different stakeholders. For example, the general public are often unaware of the signs and symptoms of AFib. Even when diagnosed, patients frequently decline therapy or have poor adherence to treatment often due to a lack of awareness or poor risk perception. Developing and supporting patient advocacy organisations may increase patient awareness of AFib, its complications and the need for appropriate treatment.
-
Experts interviewed also reported that there is a dearth of knowledge about the burden of AFib among the medical fraternity outside of heart specialists, particularly with regards to the efficacy of anticoagulant therapies, as well as the appropriate referral pathway for patients with AFib. Interviewees also reported that awareness of treatment options, such as catheter ablation, is low among primary care doctors.
- AFib-related hospitalisations are on the rise across the region. These increases are indicative of the pitfalls in AFib care. These include a lack of early intervention, suboptimal treatment as a result of inconsistent or variation in treatment strategies, poor disease management, and unsuccessful primary prevention efforts.
-
There is no universal consensus on the optimal screening mechanism for AFib, as evidenced by the diverse international recommendations on AFib screening. There is no standard protocol for AFib screening in China, India or Japan. Even in places where they do exist, such as Australia and South Korea, where single-lead ECG for screening for people aged ≥65 years is recommended, they are not implemented consistently in clinical practice. With the Asia Pacific Heart Rhythm Society’s recent publication of a three-tiered AFib screening recommendation structure, which takes into account different country characteristics, there is now a better framework for developing screening protocols in individual countries.
-
The application of digital health technologies is growing across a vast range of chronic NCDs and has great potential to enhance AFib screening. Large-scale studies in China and elsewhere have been using consumer smartwatches to screen people for AFib. Prof Guo, one of the experts interviewed as part of this research programme, led a study in China with 180,000 adults. Her team noted an abnormal heart rhythm in 0.23% of participants, and 87% of these were subsequently confirmed to have AFib – illustrating wearables' impressive ability to successfully identify people with AFib. While the experts interviewed were enthusiastic about the potential of digital health technologies for AFib, they also highlighted that referral pathways and medico-legal considerations with the use of wearables for screening need to be clearly delineated.
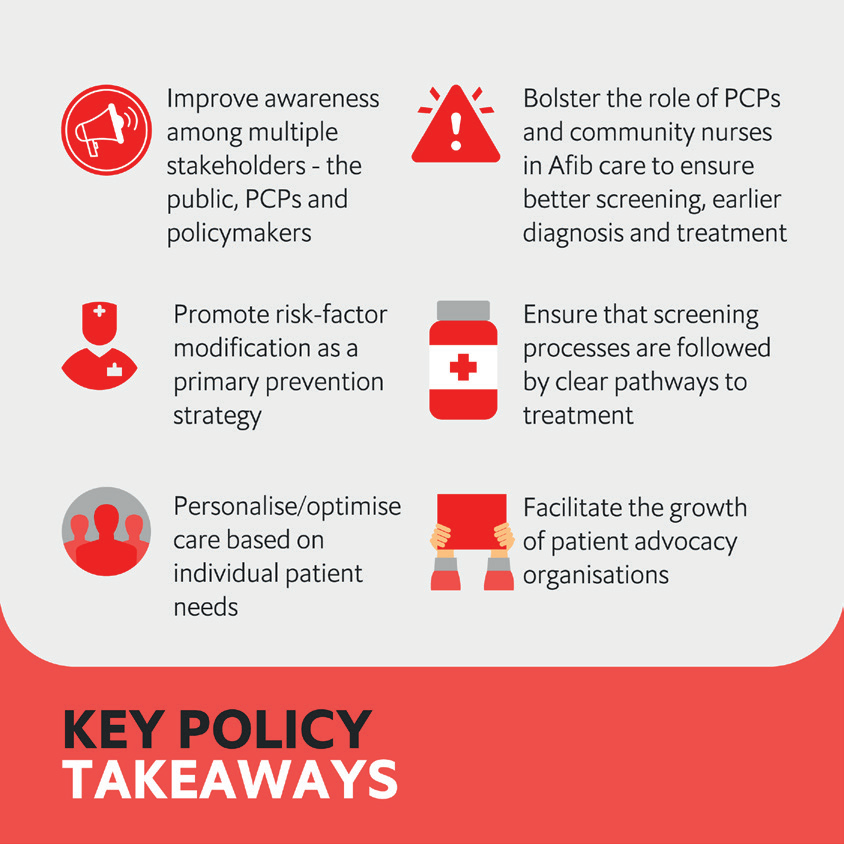
Given these insights, our research of AFib care pathways in five countries in the Asia-Pacific region has revealed six key policy takeaways: