Cancer, a leading cause of death worldwide, currently contributes to more than one in every six deaths globally. The health and economic burden posed by cancer is set to increase, with the World Health Organization (WHO) projecting that cancer incidence will increase by 50% by 2040 in comparison to 2020 levels.
The Middle East and North Africa (MENA) region is on the cusp of a demographic transition that will significantly impact the burden of cancer over the next two to three decades. The elderly population (aged 65 years) will increase by 290% between 2018 and 2050, from 28m in 2023 to 92m in 2050. As a result of the growing and ageing populations, the number of newly diagnosed cancers and cancer deaths in the WHO Eastern Mediterranean Region (EMR) is expected to double by 2040.
The rising burden of cancer will force countries to innovate, rethink strategy, and re-prioritise resources to ensure that health systems can deliver cancer care that is both high-quality and sustainable. The diversity of the MENA region in terms of population size and density, as well as economic and political systems means that the provision of, and access to, quality cancer care vary greatly across the region.
Addressing inefficiencies today is critical to safeguarding the quality of cancer care and to allowing health systems to adapt to the growing cancer burden such that they evolve for the benefit of patients and society. A number of common integrated policy priorities and interventions have been identified in this report that will help countries improve access and health outcomes in a sustainable manner.
Scale-up prevention measures – Cancer control starts with prevention. Prevention includes raising awareness of cancer, its signs and symptoms, and measures to target modifiable risk factors, such as tobacco use, physical inactivity, and unhealthy diets, which simultaneously helps to reduce the burden of other non-communicable diseases (NCDs).
Prioritise screening and early diagnosis - The majority of cancer patients in the MENA region are diagnosed in the late stages, which increases treatment costs and resources, and compromises health outcomes and survival rates. Directing healthcare spending towards screening should be an immediate policy priority because it will help support early diagnosis, thereby lowering treatment costs, while reducing the cancer mortality rate.
Strengthen end-to-end cancer services across the health system – Although tertiary cancer specialist services are available across the region, albeit with varying degrees of capacity and coverage, there is a pressing need to strengthen and integrate primary care and palliative care.
Invest in data and digital infrastructure – Deficiencies in national cancer policy, planning and programmes stem, in part, from a scarcity of data. Comprehensive data on incidence, outcomes and costs across the entire care pathway are needed to underpin investment decisions.
Collaborate to manage the economic burden and expand access – The rising costs of controlling cancer is an undeniable challenge for the MENA region. The long-term sustainability of oncology care will therefore require the collaboration of various stakeholders, including policymakers, payers, providers, industry, non-governmental organisations (NGOs), among others.
Financing reforms are crucial to sustaining equitable access and efficient use of resources – Financing reforms should also support a move from curative to preventive care, and from payment based on volume and fee-for-service models to value- and outcomes-based financing. The implementation of Health Technology Assessment (HTA) and frameworks to support economic evaluation will further support the efficient use of healthcare resources. of public funding sources.
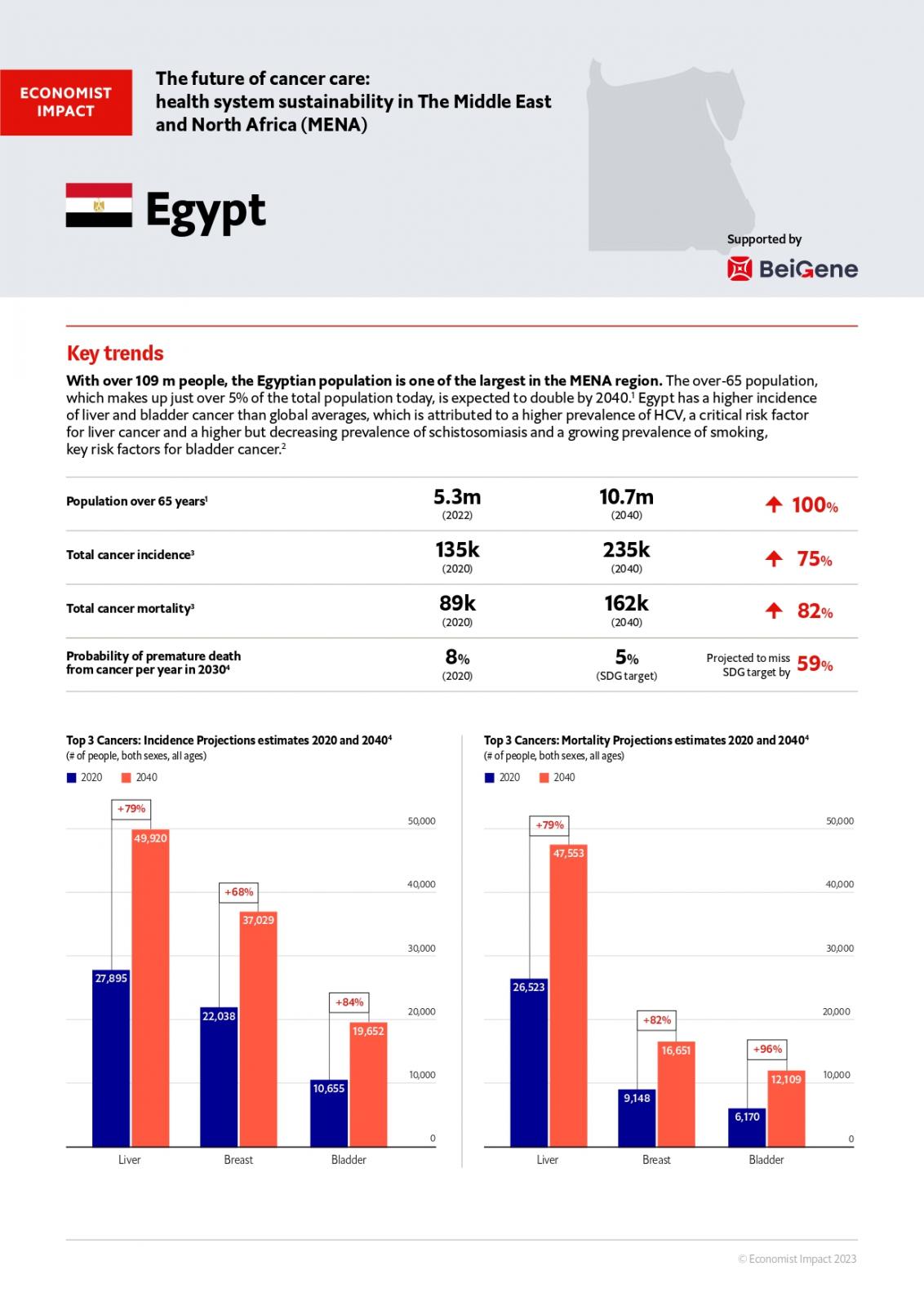
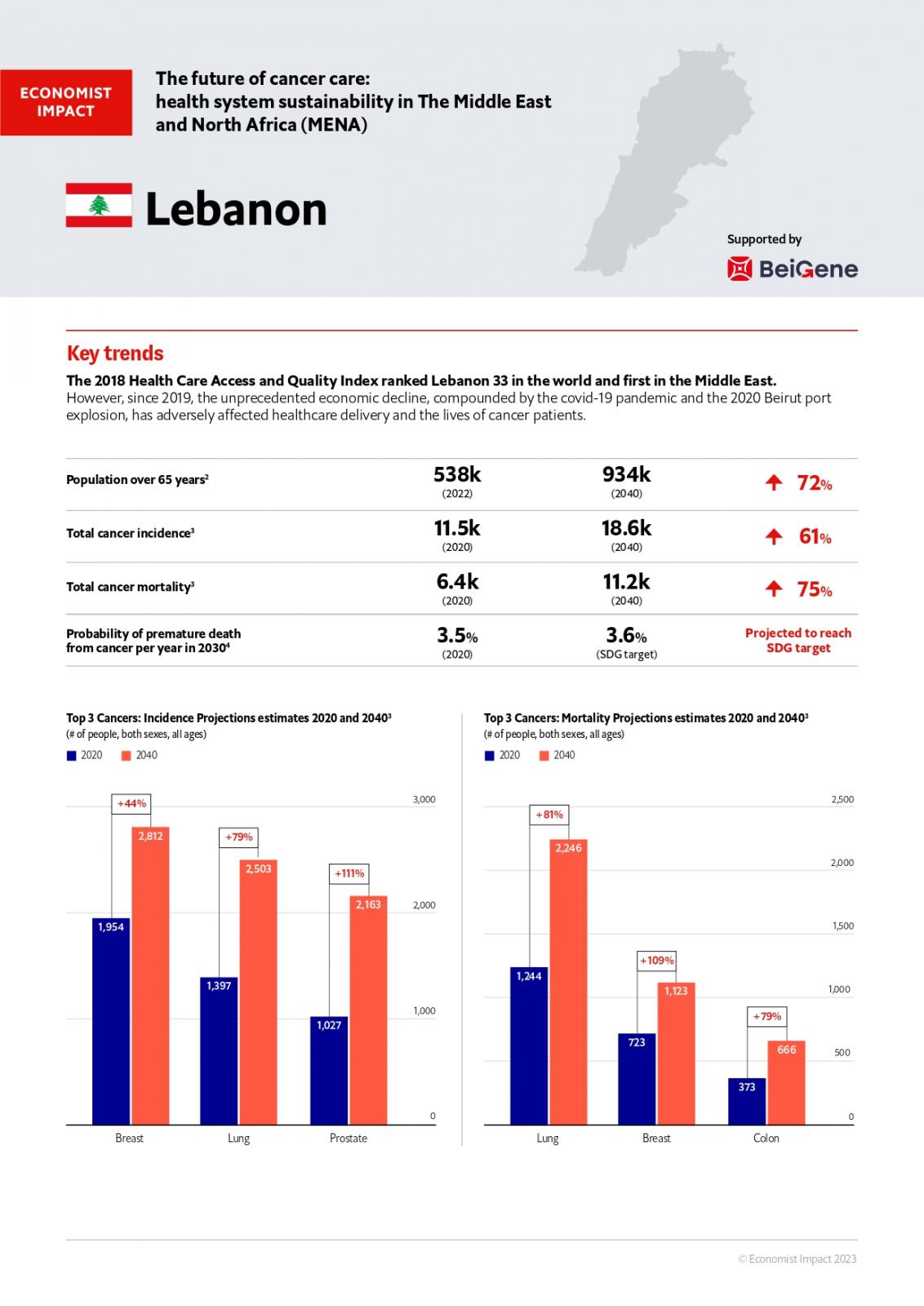
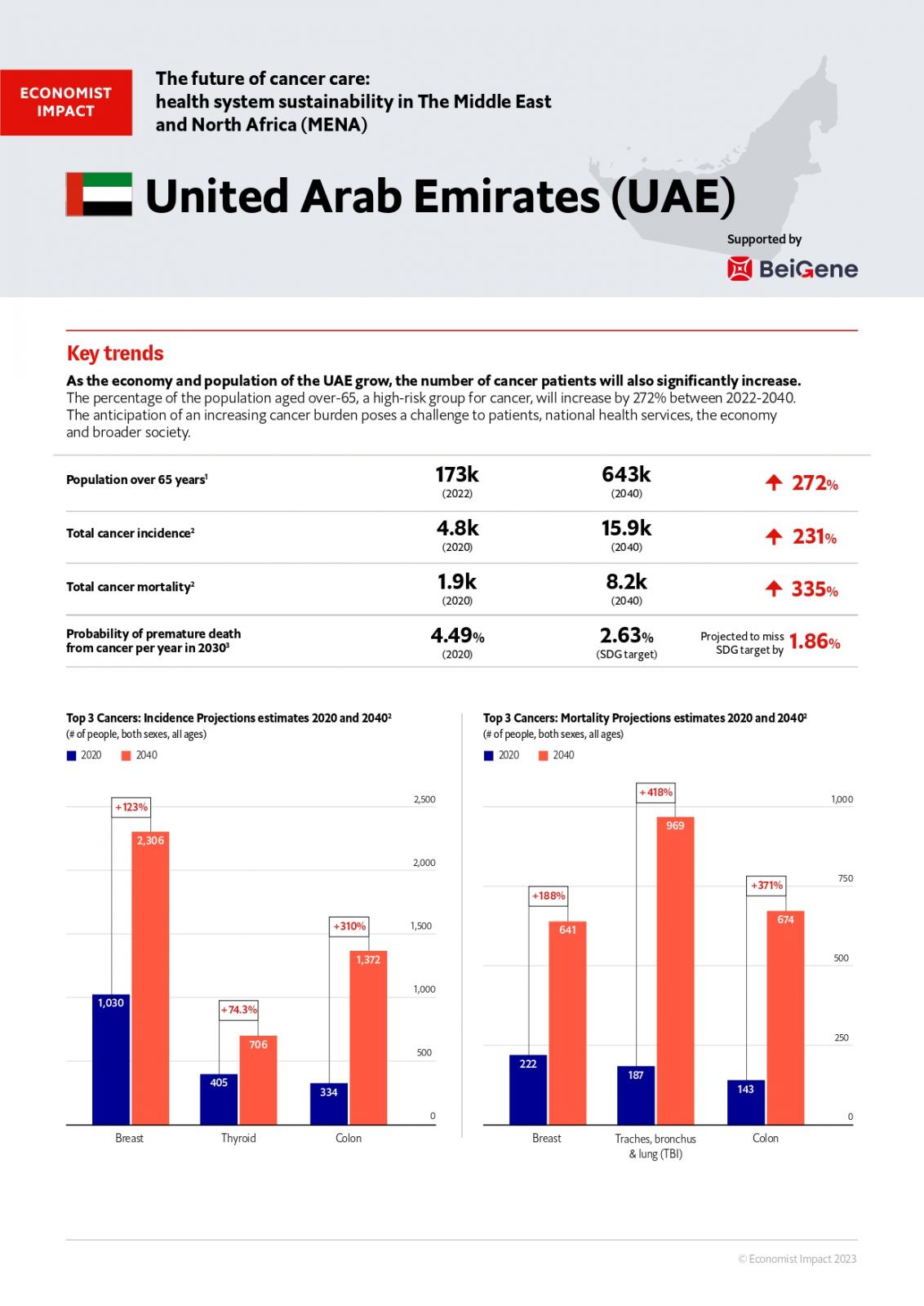
Explore our findings in the full report, alongside our country snapshots which provide an overview of the future of cancer care and health system sustainability in Egypt, Lebanon and the United Arab Emirates (UAE), along with opportunities for improvement.
Egypt
Lebanon
UAE