The health and economic burden posed by cancer is set to increase, with the World Health Organization projecting that cancer incidence will increase by 50% by 2040 when compared to 2020 levels. Of the ten most populous nations in Latin America, nine will see at least a 64% rise in the number of people diagnosed with cancer annually by 2040. In Brazil alone, this increase would mean one million newly diagnosed cancer patients needing care each year, significantly impacting its health system.
This growing burden of cancer in the region will mean that countries would need to innovate and re-prioritise resources to ensure that health systems can deliver cancer care that is both high-quality and sustainable. While the obstacles to sustainable cancer care are many, they are far from insurmountable. Given the heterogeneity of countries in the region, a one-size-fits-all approach to cancer care is unlikely to deliver optimal outcomes. However, a number of common integrated policy actions and interventions have been identified in this report to help countries in Latin America achieve greater access to, and sustainability of, oncology care.
Bridge the equity gap in the private and public health sectors – Health systems in Latin America have complex and fragmented structures that lead to inefficient delivery of care and unequal distributions of resources. A lack of equitable access to healthcare, particularly oncology care, is evident throughout the region, where socioeconomic status plays a central role in determining health outcomes. Therefore, keeping such health and healthcare inequities in mind, building a sustainable health system for oncology should begin with investing in preventive care by strengthening primary care services, expanding screening and promoting integrated care. Countries in the region also need to tackle broader societal inequities that can exacerbate cancer risk factors in order to ensure the sustainability of oncology care.
Invest in health workforce capacity-building – The region is experiencing a shortage of oncology specialists, and health systems cannot meet current demand. From radiation oncologists to palliative care specialists, creating training programs that increase the number and skills of healthcare professionals should be prioritised. Unless there is targeted investment in the capacity-building of a specialised oncology workforce, Latin America will not meet the projected increase in demand caused by the burden of cancer in the next decade. Beyond the oncology workforce, developing teams of public health workers and health personnel who deliver health-promoting activities and education will also help reduce the cancer burden and positively affect other non-communicable diseases.
Sustain and amplify innovation and technology – Data is at the core of the region's digital transformation. As many health systems digitalise, stakeholders must consider breaking down information silos created by fragmented health systems; instead data should follow patients seamlessly across the care continuum. This includes integrating, expanding and improving data collection in cancer registries. Only then will decision-makers be able to leverage data to appropriately allocate resources and formulate evidence-based policies. Stakeholders must champion the integration of evidence-based technologies and take action to update outdated policies that may hinder technological progress. Furthermore, stakeholders should also identify sustainable financing sources to support clinical trials and research involving such technologies. However, it should be noted that success in leveraging data for better health is also contingent on the regulatory environment, the quality of data security and privacy measures, and the willingness of patients and healthcare professionals to adopt technologies.
Diversity in collaboration – The primary goal of healthcare systems is to save lives and improve well-being. As such, patients should be at the centre of policy and at the forefront of decisions made by both healthcare professionals and political decision-makers. Engaging patients, advocacy and patient support groups, healthcare professionals, and community members will help provide a diverse range of perspectives and experiences, enabling policymakers or HTA committees to develop more effective policies. Furthermore, the sustainability of oncology care specifically, and healthcare as a whole, cannot be achieved by health systems alone. Health is a multidimensional concept with several determinants, including social determinants. Therefore, it requires a “Whole-of-Government” approach to improve the population’s health and lower the demand for healthcare. Keeping this in mind, countries must take a multisectoral and multi-ministerial collaborative approach to ensure the sustainability of oncology care, which has implications not just for the health of the population but for productivity and economic growth as well.
Develop a multifaceted value framework that meets local challenges and champions fairness and transparency – Establishing a systematic process to assess value comprehensively is essential to ensuring the long-term sustainability of innovations in healthcare. As systems strive to allocate resources more efficiently and move towards evidence-based decision-making, HTAs offer a systematic approach to achieving these goals. HTAs are an under-utilised approach to healthcare decision-making in Latin America. Countries must take the first step towards developing and implementing assessment frameworks through HTAs that provide more comprehensive and transparent assessments of value that extend beyond just clinical and safety data in an effort to drive greater equity and sustainability within cancer care.
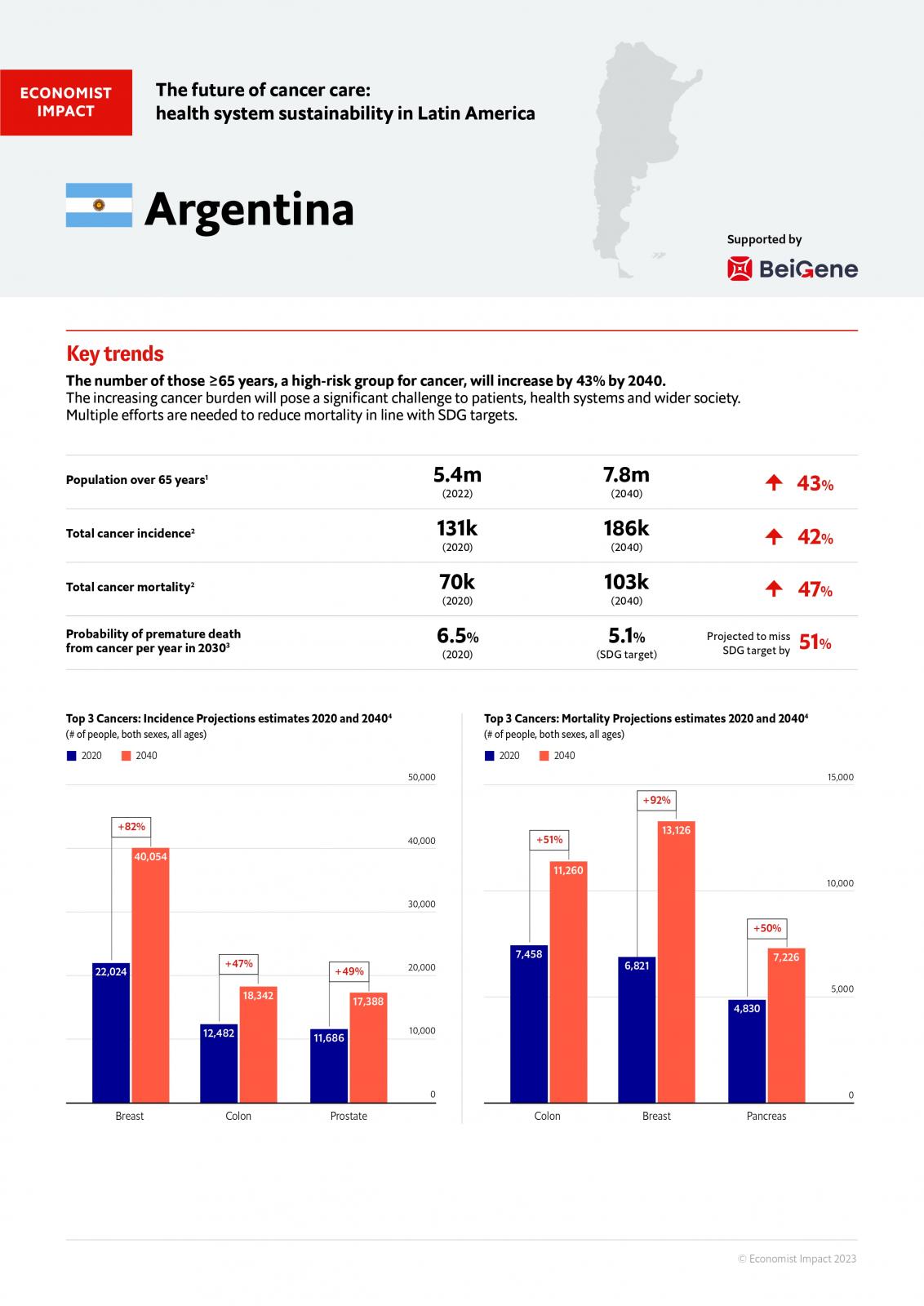
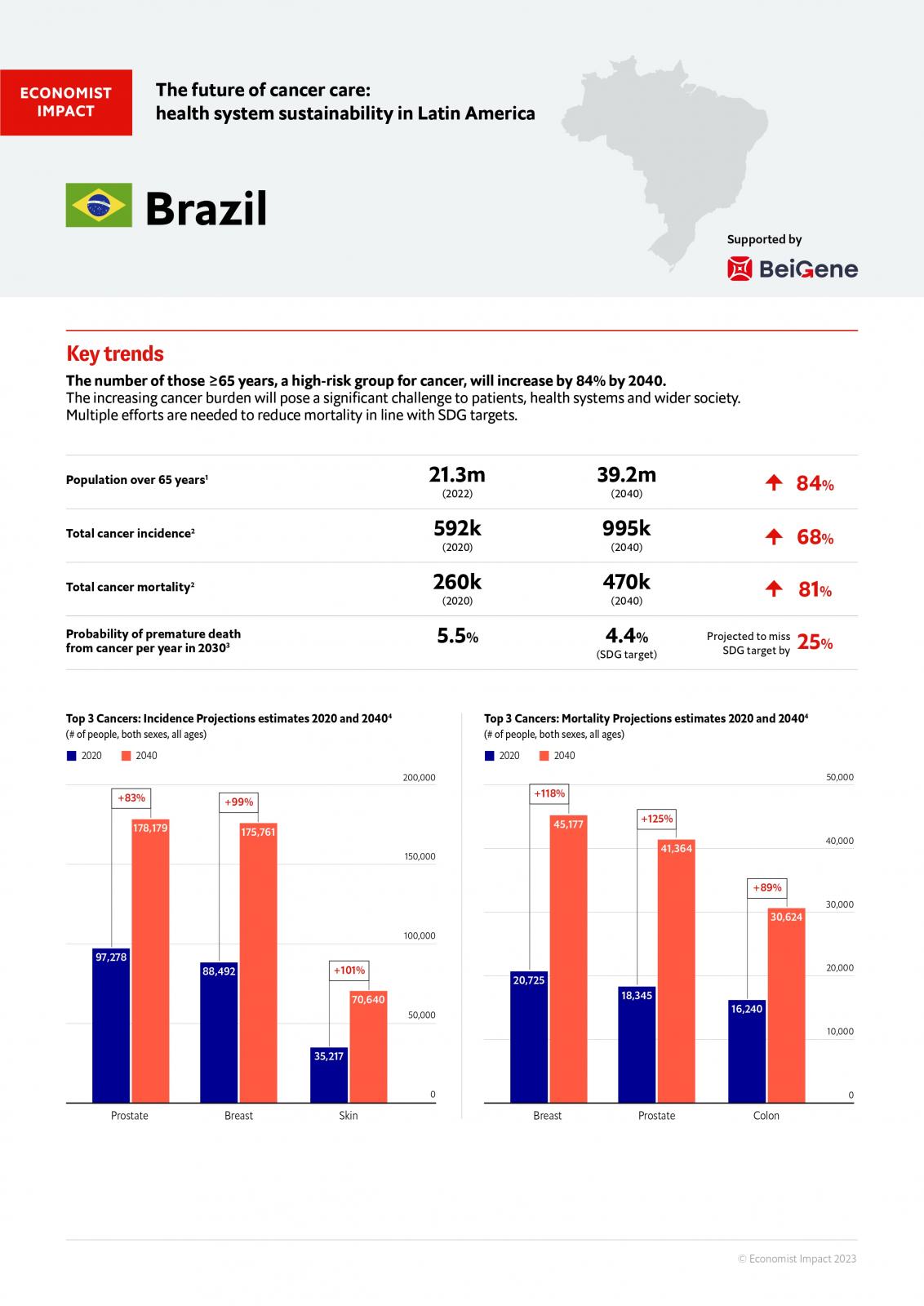
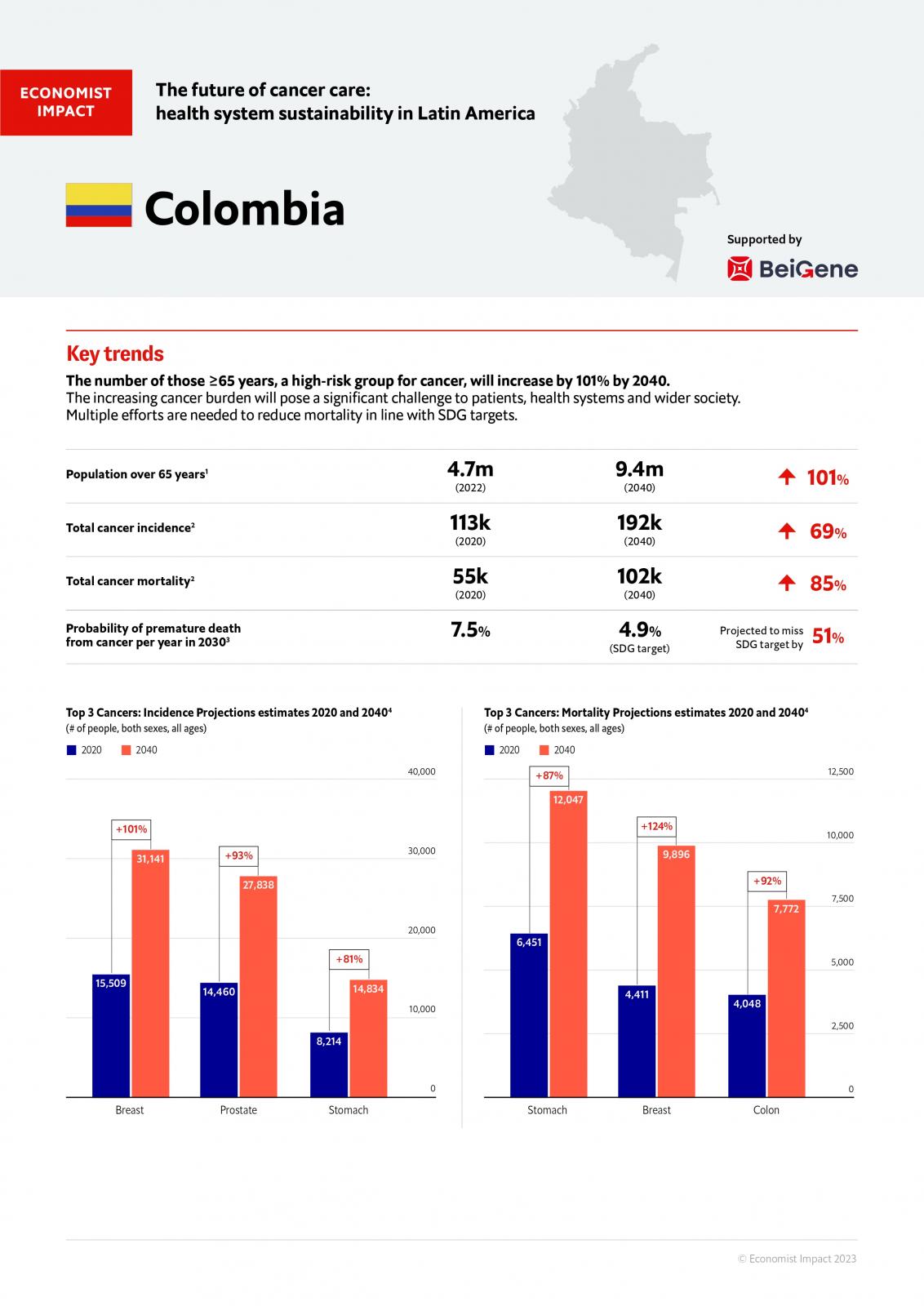
Explore our findings in the full report, alongside our country snapshots which provide an overview of the future of cancer care and health system sustainability in Argentina, Brazil and Colombia, along with opportunities for improvement.
Argentina
Brazil
Colombia